Stroke
Strokes are a highly prevalent condition that are the leading cause of chronic disability, the second leading cause of dementia (1), and the fifth leading cause of death in the US (2). Strokes occur when blood flow to a specific area of the brain is interrupted, or when a blood vessel bursts and causes bleeding in the brain. Lack of blood flow and/or brain bleeding results in brain cell death and damage, which can lead to cognitive impairments, motor issues, headaches, and vision problems (3).
Extivita Therapies for Stroke:
Extivita Therapies for Stroke Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Hyperbaric Oxygen Therapy for Stroke:
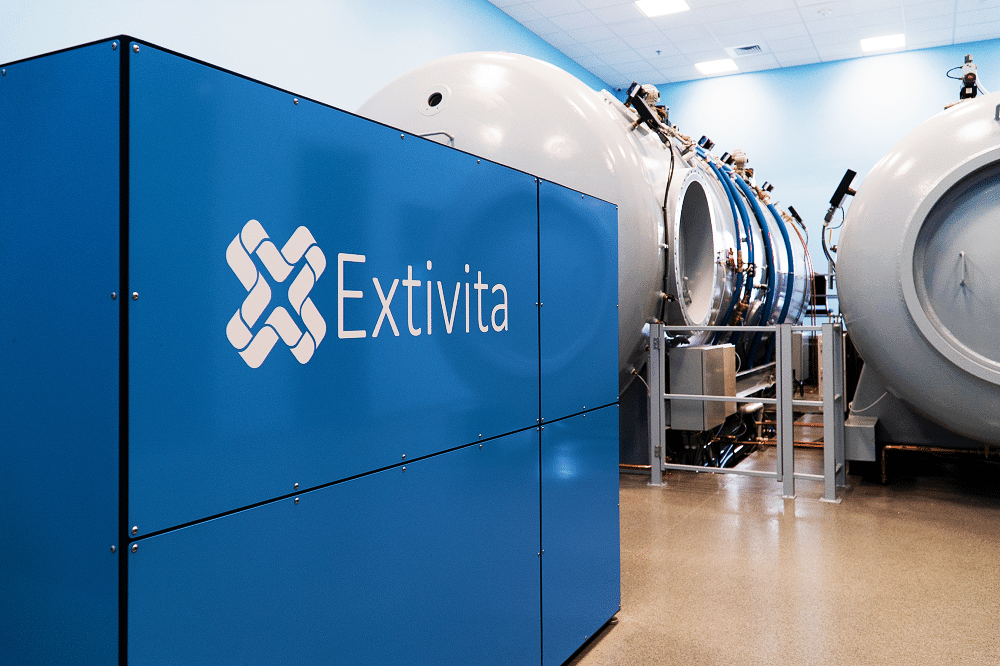
Additional studies report similar findings of improved ADLs (activities of daily living), brain metabolism, and quality of life(5,6). Brain scans showed that the damaged locations of the brain were significantly healed and reactivated in more than half of the patients(6). HBOT improves stroke symptoms by healing brain cells that were initially damaged by the stroke as well as stimulating the growth of new brain cells(4,7).
Effects of HBOT on Stroke:
New Blood Vessel Formation
Increased Stem Cell Activity

Decreased Inflammation

Neurofeedback for Stroke:
The brain has been shown to have remarkable capacity to form and reorganize synaptic connections (neuroplasticity) and recovery even in severe chronic stroke. Neurofeedback can facilitate neuroplasticity and enhance motor learning, control, memory, and cognitive function (6-7).
IV Therapy for Stroke:
Vitamin C (ascorbic acid) is an important antioxidant molecule in the body and the brain. Ascorbate (reduced form of vitamin C) scavenges free radicals, recycles other antioxidants, protects brain cells from cell damage/death. Ascorbate has been associated with neuroprotection pre- stroke, in acute stage of (and reperfusion stage), and in chronic phases of stroke (8-10). In addition, we also offer B12 with our Vitamin C infusions. B12 has been shown to enhance nerve repair (11).


Pulsed Electromagnetic Field Therapy for Stroke:
Micro vessels play a big role in overall course of vascular diseases. Dysfunction to this system has been linked to a multitude of illnesses. The PEMF device has been shown to optimize the microcirculatory system, increasing perfusion to tissues and organs. When used in conjunction with HBOT, oxygen rich blood can be delivered to these areas, where healing can begin (12).
News & Research for Stroke:
Stroke Recovery: Britney’s Recovery with HBOT
Britney Thomas's story is a testament to the power of hope, determination, and advanced medical treatment. After experiencing a life-altering stroke at a young age, Britney's journey with hyperbaric oxygen therapy (HBOT) at UAB Medicine showcases not just her personal...
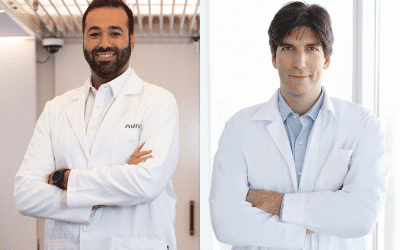
Treating chronic-stage stroke with hyperbaric oxygen therapy
Mohammed Elamir (The Villages, USA) and Amir Hadanny (Be’er Ya’akov, Israel) mark this year’s Stroke Awareness Month by discussing hyperbaric oxygen therapy (HBOT)—an emerging approach that they believe could break new ground in post-stroke recovery.Every year, more...
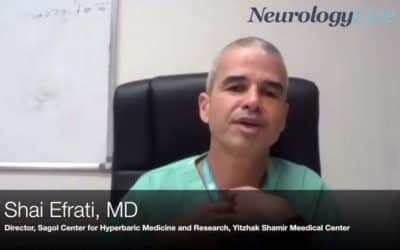
Shai Efrati, MD: Inducing Stem Cell Proliferation With Hyperbaric Oxygen Therapy
From Neurology Live. The director of the Sagol Center for Hyperbaric Medicine and Research at Yitzhak Shamir Medical Center discusses how hyperbaric oxygen therapy is being used to attempt to improve the damage from neurodegeneration.
References
- Roger, Véronique L., Alan S. Go, Donald M. Lloyd-Jones, Robert J. Adams, Jarett D. Berry, Todd M. Brown, Mercedes R. Carnethon, et al. “Heart Disease and Stroke Statistics—2011 Update.” Circulation 123, no. 4 (February 1, 2011): e18–209. https://doi.org/10.1161/CIR.0b013e3182009701.
- George, Mary G. “CDC Grand Rounds: Public Health Strategies to Prevent and Treat Strokes.” MMWR. Morbidity and Mortality Weekly Report 66 (2017). https://doi.org/10.15585/mmwr.mm6618a5.
- “Stroke: Causes, Symptoms, Diagnosis, and Treatment.” Medical News Today. Accessed June 26, 2019. https://www.medicalnewstoday.com/articles/7624.php.
- Hadanny, Amir, et al. “Hyperbaric Oxygen Therapy Improves Neurocognitive Functions of Post-Stroke Patients – a Retrospective Analysis.” Restorative Neurology and Neuroscience, vol. 38, no. 1, IOS Press, Jan. 2020, pp. 93–107. content.iospress.com, doi:10.3233/RNN-190959.
- Boussi-Gross, Rahav, et al. “Improvement of Memory Impairments in Poststroke Patients by Hyperbaric Oxygen Therapy.” Neuropsychology, vol. 29, no. 4, July 2015, pp. 610–21. PubMed, doi:10.1037/neu0000149.
- Efrati, Shai, Gregori Fishlev, Yair Bechor, Olga Volkov, Jacob Bergan, Kostantin Kliakhandler, Izhak Kamiager, et al. “Hyperbaric Oxygen Induces Late Neuroplasticity in Post Stroke Patients – Randomized, Prospective Trial.” PLOS ONE 8, no. 1 (January 15, 2013): e53716. https://doi.org/10.1371/journal.pone.0053716.
- Zhang, John H., Takkin Lo, George Mychaskiw, and Austin Colohan. “Mechanisms of Hyperbaric Oxygen and Neuroprotection in Stroke.” Pathophysiology 12, no. 1 (July 1, 2005): 63–77. https://doi.org/10.1016/j.pathophys.2005.01.003.
- Sreedharan S, Sitaram R, Paul JS, Kesavadas C. Brain-computer interfaces for neurorehabilitation. Crit Rev Biomed Eng. 2013;41(3):269-279. doi:10.1615/critrevbiomedeng.2014010697
- Kober, S.E., Schweiger, D., Witte, M. et al. Specific effects of EEG based neurofeedback training on memory functions in post-stroke victims. J NeuroEngineering Rehabil 12, 107 (2015). https://doi.org/10.1186/s12984-015–0105-6
- Harrison, Fiona E, and James M May. “Vitamin C function in the brain: vital role of the ascorbate transporter SVCT2.” Free radical biology & medicine vol. 46,6 (2009): 719-30. doi:10.1016/j.freeradbiomed.2008.12.018
- Sánchez-Moreno, Concepción et al. “Decreased levels of plasma vitamin C and increased concentrations of inflammatory and oxidative stress markers after stroke.” Stroke vol. 35,1 (2004): 163-8. doi:10.1161/01.STR.0000105391.62306.2E
- Alexandrova, Margarita & Bochev, Petyo & Markova, Vanya & Bechev, Blagovest & Popova, Marina & Danovska, Maya & Simeonova, Virginia. (2003). Oxidative stress in the chronic phase after stroke. Redox report : communications in free radical research. 8. 169-76. 10.1179/135100003225001548.
- Wu, Fangfang et al. “Vitamin B12 Enhances Nerve Repair and Improves Functional Recovery After Traumatic Brain Injury by Inhibiting ER Stress-Induced Neuron Injury.” Frontiers in pharmacology vol. 10 406. 24 Apr. 2019, doi:10.3389/fphar.2019.00406
- https://www.imin-org.eu/images/science/Haug-Report-Bemer_2016_Englisch.pdf