Alzheimer’s Disease
At Extivita, we believe integrative medicine plays a critical role in supporting cognitive health and addressing complex neurodegenerative conditions like Alzheimer’s disease. Our therapies aim to mitigate key contributors to neurodegeneration—such as inflammation, oxidative stress, reduced cerebral blood flow, and mitochondrial dysfunction—by targeting root causes and supporting brain health.
Our treatment offerings are grounded in clinical research and focus on holistic, personalized approaches. Extivita provides therapies such as Hyperbaric Oxygen Therapy (HBOT), Neurofeedback Therpay, Pulsed Electromagnetic Field (PEMF) Therapy, Nutritional IV Therapy, and Infrared Sauna, all designed to promote neurological repair, improve cognitive function, and support overall brain resilience.
Understanding Alzheimer’s
Alzheimer’s disease is the most common type of dementia, currently affecting over 6 million people in the United States. It causes a gradual decline in memory, thinking, and problem-solving skills. This decline happens as the brain begins to change—mainly due to the buildup of harmful substances like beta-amyloid plaques and tau protein tangles. Over time, these changes lead to chronic inflammation in the brain, poor energy use, and damage to the connections between brain cells.
In addition, research shows that Alzheimer’s is linked to problems with mitochondria (the energy centers of our cells) and reduced blood flow in the brain. These issues limit the delivery of oxygen and nutrients—especially to key memory areas like the hippocampus. As a result, symptoms such as memory loss, confusion, and poor judgment begin to appear and worsen over time.
At Extivita, our goal is to help repair and protect the brain by increasing oxygen levels, lowering inflammation, and delivering nutrients that support energy production, detoxification, and overall brain health.
Extivita Therapies for Alzheimer’s
Hyperbaric Oxygen Therapy

Neurofeedback

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Infrared Sauna
Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric Oxygen Therapy involves breathing 100% medical-grade oxygen in a pressurized chamber, typically at 2.0 atmospheres absolute (ATA). This hyperoxic environment significantly increases plasma oxygen levels, promoting oxygen delivery to the brain’s tissues—even in areas with impaired blood flow. In Alzheimer’s, this improved oxygenation may help restore function in brain regions affected by poor circulation and support cognitive health.
In the context of Alzheimer’s Disease, HBOT
Improves Cerebral Blood Flow
HBOT has been shown to increase angiogenesis (formation of new capillaries), especially in ischemic areas of the brain. Improved perfusion may enhance cognitive function and memory by restoring nutrient and oxygen delivery to damaged areas.
Reduces Neuroinflammation
HBOT lowers harmful inflammation in the brain by reducing chemicals like TNF-α and IL-1β. These chemicals activate brain cells that, when overactive, can damage neurons and make memory and thinking worse. Calming this process may help protect brain cells and slow down Alzheimer’s progression.
Enhances Mitochondrial Function
HBOT increases oxygen in the brain, helping mitochondria produce more ATP—our cells’ energy source. In Alzheimer’s, energy production is often low, which affects memory and thinking. More energy helps brain cells communicate, repair damage, and function better.
Activates Stem Cells for Brain Repair
HBOT has been shown to activate neural stem cells, which can turn into new brain cells and support the repair of damaged tissue. In Alzheimer’s, brain cell loss and shrinkage are common. By promoting stem cell activity, HBOT may help replace lost neurons, improve brain structure, and support memory and cognitive function over time.
Stimulates Neurogenesis and Plasticity
HBOT may help grow new brain cells—especially in the hippocampus, the area linked to memory. It also supports brain plasticity, which is the brain’s ability to form new connections. This can help improve learning, memory, and overall brain function in people with Alzheimer’s.
Neurofeedback Therapy
Neurofeedback is a non-invasive brain training technique that uses real-time EEG monitoring to help individuals regulate and optimize brain wave activity. It is based on operant conditioning, where the brain learns to produce healthier patterns associated with focus, calm, and cognitive clarity. In Alzheimer’s, brain waves can become irregular, contributing to confusion, memory loss, and poor attention. By training the brain to return to more balanced activity, neurofeedback may help improve mental clarity, reduce agitation, and support daily cognitive function.
Neurofeedback Therapy Supports Alzheimer’s in Several Ways
Improves Brainwave Regulation
Neurofeedback helps the brain move away from unhealthy brainwave patterns—like too much delta or theta activity—which are common in people with memory loss or confusion. These slow waves can make it harder to focus, stay alert, or process information. By encouraging more balanced and active brainwaves, neurofeedback may help improve attention, clarity, and overall brain performance in individuals with Alzheimer’s.
Enhances Memory and Focus
Neurofeedback may strengthen areas of the brain responsible for memory, attention, and decision-making—skills that often decline in the early stages of Alzheimer’s. By improving how these brain regions communicate, individuals may experience sharper focus, better recall, and improved ability to complete everyday tasks.
Supports Neuroplasticity
Neurofeedback helps the brain build new and stronger connections by encouraging healthy brainwave patterns. This process, called neuroplasticity, allows the brain to adapt and rewire itself, which is especially important for slowing down the cognitive decline seen in Alzheimer’s disease.

Reduces Anxiety and Sleep Disturbances
People with Alzheimer’s often struggle with anxiety and poor sleep, which can make symptoms worse. Neurofeedback helps calm overactive brain patterns linked to stress and encourages brain states that promote deeper, more restful sleep—helping improve mood, energy, and mental clarity.
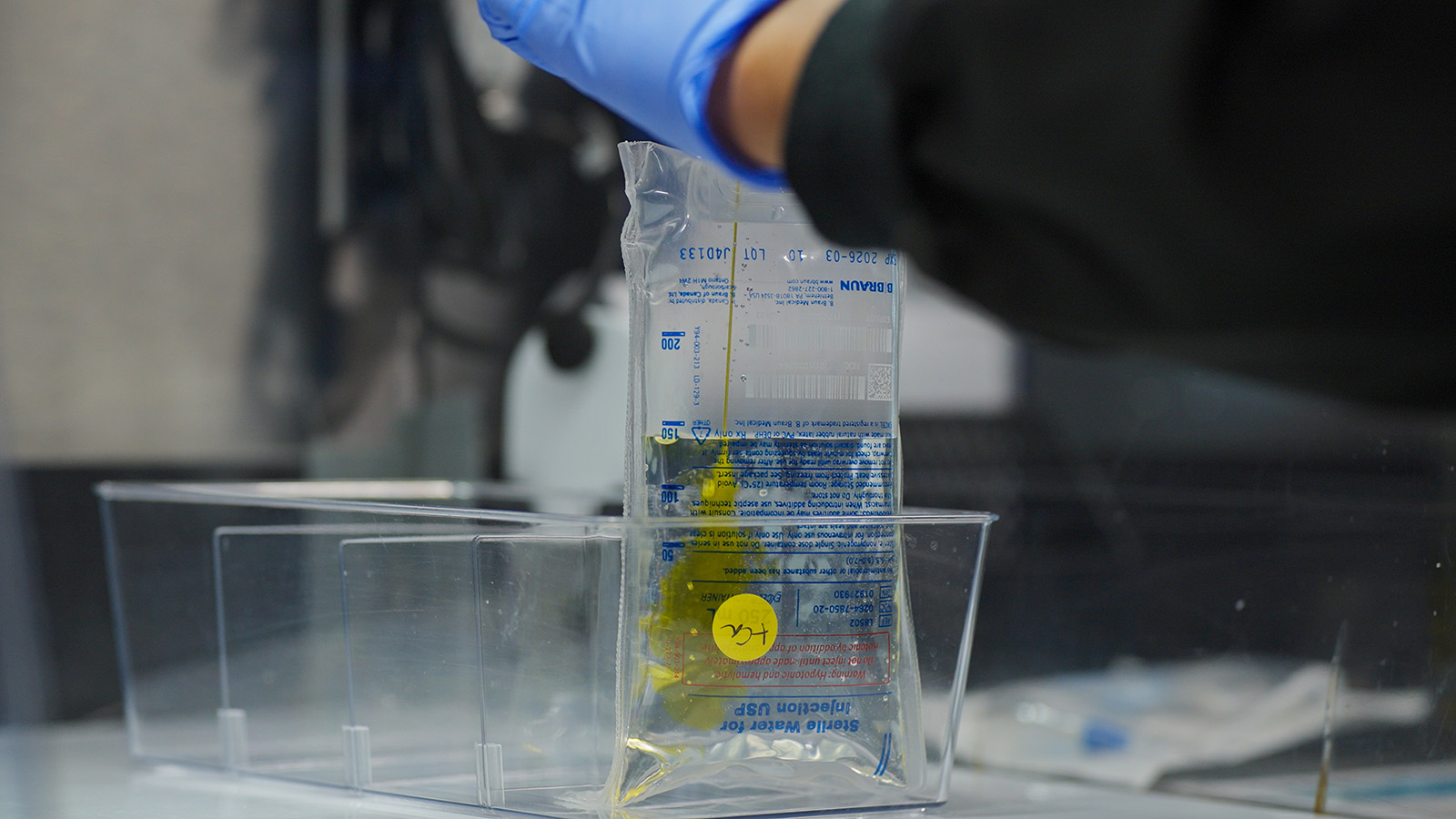
Nutritional IV Therapy
Nutritional IV Therapy delivers high concentrations of brain-supportive nutrients directly into the bloodstream. This bypasses the gastrointestinal system, allowing for rapid absorption and cellular uptake—particularly important in individuals with impaired nutrient metabolism or absorption. In Alzheimer’s, this can help address common nutritional deficiencies that contribute to cognitive decline and support overall brain function.
Nutritional IV Therapy Supports Alzheimer’s in Several Ways

Neuroprotection & Antioxidant Support
Nutrients like Glutathione and Vitamin C neutralize free radicals that contribute to neuronal damage in Alzheimer’s. These antioxidants help reduce oxidative stress, a major driver of memory loss and brain cell aging in Alzheimer’s patients.
Mitochondrial Support
B vitamins and Magnesium support mitochondrial energy production, helping sustain cognitive function. In Alzheimer’s disease, mitochondrial dysfunction is a key feature that contributes to neuronal death and cognitive decline; thus, supporting mitochondrial health may help preserve memory, reduce neurodegeneration, and improve overall brain resilience.
Reduces Oxidative Stress
Glutathione plays a critical dual role in brain health by neutralizing oxidative stress—an imbalance between free radicals and antioxidants that damages neurons—and aiding in the removal of heavy metals and neurotoxins that impair cognitive function. This is especially important for individuals with Alzheimer’s disease, where elevated oxidative stress and accumulation of neurotoxic substances contribute to neurodegeneration
Recommended IV Therapies
Myers’ Cocktail
Components: B complex vitamins, Vitamin C, Magnesium, Calcium
• B-vitamins support neurotransmitter synthesis and cognitive function
• Vitamin C helps reduce oxidative damage
• Magnesium modulates NMDA receptor activity, protecting against excitotoxicity
Glutathione IV
Components: Reduced Glutathione
• Supports detoxification and reduces neuroinflammation
• Shown to preserve mitochondrial function and slow cognitive decline
Hydration IV
Components: Normal Saline (500mL or 1000 mL)
- Maintains fluid balance and supports metabolic processes essential for brain health
NAD+ Trio
Components: NAD+, Myers’ Cocktail, Glutathione
- Supports mitochondrial energy production, enhances cellular repair, and reduces neuroinflammation—key factors in protecting brain cells and slowing cognitive decline in Alzheimer’s disease.
Pulsed Electromagnetic Field (PEMF) Therapy
PEMF Therapy uses low-frequency electromagnetic waves to gently stimulate the body’s cells. This non-invasive treatment may enhance circulation, support energy delivery at the cellular level, and promote overall wellness. PEMF therapy may benefit individuals with Alzheimer’s disease by improving microcirculation in the brain, enhancing mitochondrial function, and supporting neural repair, potentially slowing cognitive decline.
How PEMF Therapy Supports Alzheimer’s
Enhances Microcirculation
PEMF increases capillary blood flow in the brain, which may improve oxygen and nutrient delivery to neurons. Improved cerebral microcirculation enhances the delivery of glucose and essential compounds needed for neurotransmitter synthesis and cellular repair. In Alzheimer’s disease, where reduced cerebral blood flow is commonly observed and linked to accelerated cognitive decline, enhancing microvascular circulation may help protect neurons, support synaptic activity, and slow disease progression.
Reduction in Neuroinflammation
PEMF therapy helps calm inflammation in the brain by lowering harmful substances called inflammatory cytokines—such as TNF-α, IL-1β, and IL-6. These are often elevated in people with Alzheimer’s disease and can damage brain cells over time. PEMF also helps regulate microglia, the brain’s immune cells. When overactive, microglia can harm neurons, but PEMF encourages them to switch to a more protective, healing state. By reducing this chronic inflammation, PEMF may help slow the progression of Alzheimer’s, protect brain cells, and support memory and thinking.
Reduces Oxidative Stress
Glutathione plays a critical dual role in brain health by neutralizing oxidative stress—an imbalance between free radicals and antioxidants that damages neurons—and aiding in the removal of heavy metals and neurotoxins that impair cognitive function. This is especially important for individuals with Alzheimer’s disease, where elevated oxidative stress and accumulation of neurotoxic substances contribute to neurodegeneration.
Infrared Sauna
Infrared Sauna Therapy utilizes infrared light to gently heat the body directly, rather than warming the air around you. This method allows for a more comfortable experience at lower temperatures compared to traditional saunas, typically operating between 120°F and 140°F (49°C and 60°C). The deep-penetrating heat may promote relaxation and support overall wellness.
How Infrared Sauna Supports Alzheimer’s
Enhanced Circulation
Infrared sauna therapy gently raises the body’s core temperature, which naturally increases heart rate and widens blood vessels—boosting circulation throughout the body, including the brain. Improved blood flow enhances oxygen and nutrient delivery to brain cells, which is vital for memory, focus, and overall cognitive function.
Stress Reduction
Regular sessions can promote relaxation and reduce stress levels, which is beneficial for hormonal balance and overall reproductive health.

Detoxification
Infrared therapy promotes sweating, facilitating the elimination of neurotoxic metals like mercury, aluminum, and lead, which are linked to cognitive decline.
Ready to Support Your Brain Health?
At Extivita, we understand that Alzheimer’s disease presents significant emotional and physical challenges. Our approach focuses on addressing root causes of cognitive decline—like inflammation, oxidative stress, and impaired blood flow—using therapies that promote cellular repair, energy production, and detoxification.
Schedule a free wellness consultation to explore a personalized plan that supports your cognitive health and overall brain function.
Medical Disclaimer
The therapies discussed on this page are not FDA-approved for the treatment of Alzheimer’s disease. They are offered as complementary wellness therapies and should not replace advice from your neurologist or primary healthcare provider. Results may vary by individual.
Schedule Your Free Wellness Visit →
References:
- Somaa, Fahad. “A review of the application of hyperbaric oxygen therapy in alzheimer’s disease.” Journal of Alzheimer’s Disease, vol. 81, no. 4, 15 June 2021, pp. 1361–1367, https://doi.org/10.3233/jad-210157.
- Le, Wei-Dong, et al. “The neuroprotective effects of oxygen therapy in alzheimer’s disease: A narrative review.” Neural Regeneration Research, vol. 18, no. 1, 25 Apr. 2022, p. 57, https://doi.org/10.4103/1673-5374.343897.
- “HBOT Showed Improvement in Alzheimer’s Disease.” LSU Health, LSU Health, www.lsuhsc.edu/newsroom/HBOT%20Showed%20Improvement%20in%20Alzheimer%E2%80%99s%20Disease.html#:~:text=After%2040%20treatments%2C%20she%20reported,a%20recurrence%20in%20her%20symptoms. Accessed 19 June 2025.
- Marcinkowska, Anna B., et al. “Impact of hyperbaric oxygen therapy on cognitive functions: A systematic review.” Neuropsychology Review, vol. 32, no. 1, 13 Apr. 2021, pp. 99–126, https://doi.org/10.1007/s11065-021-09500-9.
- Gottfried, Irit, et al. “Hyperbaric oxygen treatment—from mechanisms to cognitive improvement.” Biomolecules, vol. 11, no. 10, 15 Oct. 2021, p. 1520, https://doi.org/10.3390/biom11101520.
- Tatar, Selçuk, et al. “Hyperbaric oxygen therapy for five days increases blood-brain barrier permeability.” Undersea and Hyperbaric Medicine, vol. 44, no. 4, 1 July 2017, pp. 345–355, https://doi.org/10.22462/7.8.2017.7.
- Toda, Tomohisa, et al. “The role of adult hippocampal neurogenesis in brain health and disease.” Molecular Psychiatry, vol. 24, no. 1, 20 Apr. 2018, pp. 67–87, https://doi.org/10.1038/s41380-018-0036-2.
- Bin-Alamer, Othman, et al. “Hyperbaric oxygen therapy as a neuromodulatory technique: A review of the recent evidence.” Frontiers in Neurology, vol. 15, 9 Oct. 2024, https://doi.org/10.3389/fneur.2024.1450134.
- Huang, Xu, et al. “Hyperbaric oxygen potentiates diabetic wound healing by promoting fibroblast cell proliferation and endothelial cell angiogenesis.” Life Sciences, vol. 259, 15 Oct. 2020, p. 118246, https://doi.org/10.1016/j.lfs.2020.118246.
- Gottfried, Irit, et al. “Hyperbaric oxygen treatment—from mechanisms to cognitive improvement.” Biomolecules, vol. 11, no. 10, 15 Oct. 2021, p. 1520, https://doi.org/10.3390/biom11101520.
- Thom, Stephen R., et al. “Stem cell mobilization by Hyperbaric Oxygen.” American Journal of Physiology-Heart and Circulatory Physiology, vol. 290, no. 4, 1 Apr. 2006, https://doi.org/10.1152/ajpheart.00888.2005.
- Srivastava, Sarika. “The mitochondrial basis of aging and age-related disorders.” Genes, vol. 8, no. 12, 19 Dec. 2017, p. 398, https://doi.org/10.3390/genes8120398.
- Schottlender, Nofar, et al. “Hyperbaric oxygen treatment: Effects on mitochondrial function and oxidative stress.” Biomolecules, vol. 11, no. 12, 3 Dec. 2021, p. 1827, https://doi.org/10.3390/biom11121827.
- Loriette, C., et al. “Neurofeedback for cognitive enhancement and intervention and brain plasticity.” Revue Neurologique, vol. 177, no. 9, 19 Oct. 2021, pp. 1133–1144, https://doi.org/10.1016/j.neurol.2021.08.004.
- Quevedo, Karina, et al. “Neurofeedback and neuroplasticity of visual self-processing in depressed and healthy adolescents: A preliminary study.” Developmental Cognitive Neuroscience, vol. 40, Dec. 2019, p. 100707, https://doi.org/10.1016/j.dcn.2019.100707.
- Gu, Yue, et al. “Improving attention through individualized fnirs neurofeedback training: A pilot study.” Brain Sciences, vol. 12, no. 7, 29 June 2022, p. 862, https://doi.org/10.3390/brainsci12070862.
- Jiang, Yang, et al. “Sharpening working memory with real-time electrophysiological brain signals: Which neurofeedback paradigms work?” Frontiers in Aging Neuroscience, vol. 14, 28 Mar. 2022, https://doi.org/10.3389/fnagi.2022.780817.
- Chen, Chao, et al. “Efficacy evaluation of neurofeedback-based anxiety relief.” Frontiers in Neuroscience, vol. 15, 28 Oct. 2021, https://doi.org/10.3389/fnins.2021.758068
- Vilou, Irini, et al. “EEG-neurofeedback as a potential therapeutic approach for cognitive deficits in patients with dementia, multiple sclerosis, stroke and Traumatic Brain Injury.” Life, vol. 13, no. 2, 29 Jan. 2023, p. 365, https://doi.org/10.3390/life13020365.
- Campbell, Jared M. “Supplementation with NAD+ and its precursors to prevent cognitive decline across disease contexts.” Nutrients, vol. 14, no. 15, 7 Aug. 2022, p. 3231, https://doi.org/10.3390/nu14153231.
- Wang, Xinshi, et al. “NAD+ in alzheimer’s disease: Molecular mechanisms and systematic therapeutic evidence obtained in vivo.” Frontiers in Cell and Developmental Biology, vol. 9, 3 Aug. 2021, https://doi.org/10.3389/fcell.2021.668491.
- Aoyama, Koji. “Glutathione in the brain.” International Journal of Molecular Sciences, vol. 22, no. 9, 9 May 2021, p. 5010, https://doi.org/10.3390/ijms22095010.
- Peng, Lihong, et al. “The effect of pulsed electromagnetic fields on angiogenesis.” Bioelectromagnetics, vol. 42, no. 3, 6 Mar. 2021, pp. 250–258, https://doi.org/10.1002/bem.22330.
- Capelli, Enrica, et al. “Low-frequency pulsed electromagnetic field is able to modulate mirnas in an experimental cell model of alzheimer’s disease.” Journal of Healthcare Engineering, vol. 2017, 2 May 2017, pp. 1–10, https://doi.org/10.1155/2017/2530270.
- Ross, Christina L., et al. “The use of pulsed electromagnetic field to modulate inflammation and improve tissue regeneration: A Review.” Bioelectricity, vol. 1, no. 4, 1 Dec. 2019, pp. 247–259, https://doi.org/10.1089/bioe.2019.0026.
- Urban Float. “BUS Study: How Infrared Saunas Can Help You Detox Heavy Metals.” Urban Float, https://www.urbanfloat.com/blog/bus-study-infrared-saunas-are-a-powerful-detox-tool
- Chang, Ming, et al. “A study on neural changes induced by sauna bathing: Neural basis of the ‘Totonou’ State.” PLOS ONE, vol. 18, no. 11, 27 Nov. 2023, https://doi.org/10.1371/journal.pone.0294137.