Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) harnesses the benefits of elevated pressure and 100% medical-grade oxygen to heal your entire body from the inside out. It’s effects on blood flow, gene expression, and countless other physiological systems make HBOT an effective therapy for both acute and chronic health concerns.
Why Hyperbaric Oxygen Therapy?
Hyperbaric Oxygen Therapy, or “HBOT,” involves breathing 100% oxygen in a pressurized chamber to significantly increase oxygen supply to your cells and tissues. The effects this has on your body makes HBOT incredibly beneficial for a wide range of indications for everything from post-COVID brain fog and concussions, to post-surgical healing and even dementia. HBOT has such a large therapeutic range because of the positive changes it induces on several key systems; especially the circulatory, immune, and regenerative systems.
In most medical conditions, one or more biological systems are dysfunctional and contribute to disease symptoms and progression. For example, the immune system is compromised in conditions such as Crohn’s disease while the circulatory system is dysfunctional in conditions such as dementia. By targeting the majority of these systems, HBOT can effectively improve a wide range of conditions as well as general health and wellbeing.
A century of clinical research has shown that the combination of oxygen and pressure:
- Increase levels of oxygen in your blood plasma, accelerating our natural ability to heal
- Regulates 8,101 of approximately 20,000 total genes
- Upregulates anti-inflammatory genes
- Down regulated inflammatory genes
- Mobilizes stem cells and growth factors associated with the body’s regenerative and reparative processes
Request More Information:
Who can Hyperbaric Oxygen Therapy Help?
HBOT can be used to treat countless medical conditions (both on and off label), accelerate recovery from acute injuries, protect against age-related diseases, and improve general health and wellness. Below are some of the most common conditions we see here at Extivita for HBOT.
For a comprehensive list of conditions please visit our conditions we treat page.
What is Hyperbaric Oxygen Therapy?
HBOT involves sitting in a hyperbaric chamber while breathing 100% medical grade oxygen through a mask or hood. The hyperbaric chamber gradually pressurizes to between 1.5 and 2.5 times the normal atmospheric pressure (referred to as 1.5 ATA and 2.5 ATA). This is equivalent to diving between 16 feet (1.5 ATA) and 50 feet (2.5 ATA) below water.
The majority of HBOT treatments at Extivita are at 2.0 ATA, which is equivalent to 33 feet below surface level. Because oxygen is considered a drug by the FDA, patients must obtain a prescription from a licensed healthcare professional for these therapeutic treatments. The specific pressure is also included in the prescription. Our in-clinic Nurse practitioner can write HBOT prescriptions following your in-person consultation.
How does Hyperbaric Oxygen Therapy Work?
Our cells need oxygen to heal and stay healthy, and HBOT increases oxygen levels in the body by up to 1200% during treatments. In the hyperbaric chamber, patients breathe 100% medical-grade oxygen at an elevated atmospheric pressure, which allows the blood to “carry” and transport much higher concentrations of oxygen to our tissues(1).
Such an increase in oxygen causes elevated production of reactive oxygen species (ROS) and reactive nitrogen species (RNS). Both ROS’s and RNS’s have been shown to regulate thousands of genes that control growth factors, cytokines, and hormones, and more(2, 3). HBOT can regulate these genes in a way that reduces inflammation, increases stem cell availability, forms new blood vessels, and defends against bacteria(3, 4).
New Blood Vessel Formation
Hyperbaric Oxygen Therapy (HBOT) has been shown to stimulate the formation of new blood vessels via processes called angiogenesis and vasculogenesis(5). In angiogenesis, HBOT increases the synthesis of growth factors that cause existing cells to form new blood vessels(6). In vasculogenesis, HBOT increase causes the formation of completely new blood vessels by mobilizing stem cells from the bone marrow(5). New blood vessels help transport nutrients and oxygen to injured tissue and facilitate healing which otherwise might not have taken place.
Increased Stem Cell Activity
A stem cell has the potential to develop into nearly any type of cell in the body, providing the body with an innate regenerative system. HBOT increases the proliferation and release of stem progenitor cells (SPC’s) from bone marrow to peripheral circulation(8, 9). Such SPC’s induce the growth of new blood vessels (angiogenesis) for tissue repair, health, and regeneration(7). Increasing SPC activity is crucial for the treatment of degenerative and inherited diseases(10,11).
Decreased Inflammation
In many diseases, the body responds to physiological issues by increasing its inflammatory response. Although this is necessary to some extent, certain cytokines (such as IL-1, IL-6) can cause serious problems when over-produced(12). Hyperbaric oxygen therapy (HBOT) has been shown to decrease systemic inflammation in the body(13). Research has demonstrated that HBOT does this by increasing the expression of anti-inflammatory genes and decreasing the expression of inflammatory genes(12,14). This results in a lowered inflammatory response that prevents further tissue damage and facilitates healing of inflamed tissue.
Antibacterial & Antimicrobial
Hyperbaric Oxygen Therapy (HBOT) is known to increase the presence of reactive oxygen species (ROS), molecules which have a direct antimicrobial effect on certain bacteria(15). Elevated ROS’s damage the cellular components of such bacteria, and ultimately eliminate the conditions which bacteria require to live(16). The high oxygen tension reached during HBOT also prevents disease-causing microorganisms from surviving. Lastly, HBOT has also been shown to improve the effects of certain antibiotics on infected tissues, suggesting its use as an adjunct treatment to conventional antibiotic medications(17,18).
Frequently Asked Questions About Hyperbaric Oxygen Therapy
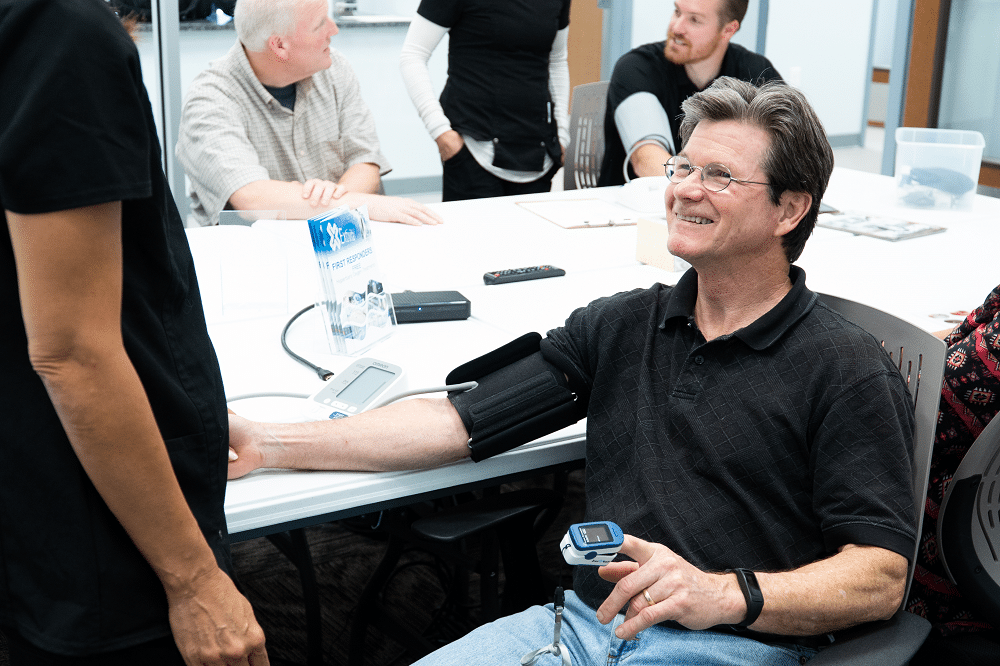
How do I get started with HBOT (new patients)?
Before you come into the clinic, you will need to register as a patient in our patient portal. Here you will enter your medical history and primary reason(s) for starting HBOT. When you complete the portal registration, you will then be able to schedule a consultation with Elena Schertz, FNP to obtain your oxygen prescription. Because oxygen is considered a drug by the FDA, patients must obtain a prescription from a licensed healthcare professional for these therapeutic treatments. The specific pressure for your HBOT treatment is also included in the prescription.
After the consultation, your HBOT journey begins!
Review our Welcome Letter for more information.
How is HBOT administered?
All Extivita patients have their very own hood or mask through which 100% medical grade oxygen is administered. These will be provided after your consultation.
The combination of oxygen and pressure is what creates a Hyperbaric Oxygen Therapy environment. The majority of our dives at Extivita are at a 2.0 ATA, which is the equivalent of being 33 feet below surface level; hence why the industry uses the term “dive” when referring to a HBOT treatment.
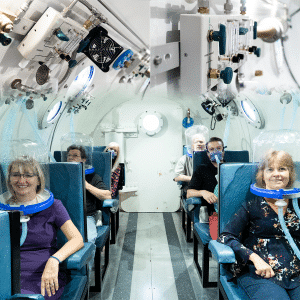
What type of HBOT chambers do we use?
At Extivita we have two hard-shell, multi-place chambers. Our biggest chamber can seat up to 12 patients, while our smaller chamber can seat up to 8 patients. We are a NFPA compliant facility; meeting all necessary safety rules and PVHO mandates required for clinical HBOT operation in North Carolina.
It’s important to know there are two types of chambers (hard and soft shell) that administer HBOT in the Health & Wellness industry. There are physical and therapeutic differences between them both, and different states enforce different mandates. In North Carolina, the PVHO (Pressure Vessels for Human Occupancy) mandate is enforced for every operational clinical hyperbaric chamber in the state. Mild HBOT or mHBOT chambers that are “soft-sided” are not compliant with ASME PVHO-1 or NFPA 99.
To learn more on the importance of this information, reference –
What is the Difference Between Hard & Soft Shell HBOT Chambers
Why PVHO Mandates are Enforced in 11 States for Hyperbaric Oxygen Therapy
What can I do while in the HBOT chamber?
Whether it’s reading, watching a movie, or sleeping, there is plenty to do during your HBOT session. All of our chambers have a tablet at each seat, and we provide free chamber-approved headphones! If you want to watch movies or shows on your personal streaming account (like Netflix, Disney+, etc), just be sure you have your login information handy. You are also more than welcome to bring your own book to read during treatment, or a small pillow for catching up on some sleep. We provide blankets to all patients.
No newspapers or cell phones are allowed in the HBOT chambers
Will I be by myself during my HBOT session?
There will always be a trained Extivita dive tender with you during your HBOT session. While you may be the only patient in the chamber on some days, most sessions will have other patients in the chamber with you.
How long does an HBOT session last?
Most HBOT sessions will last roughly 1 hour and 30 minutes, which includes the time it takes to pressurize the chamber, 1 hour at the prescribed depth, and the time it takes to depressurize the chamber. Certain conditions may require shorter or longer durations at depth.
What is a covered versus a non-covered condition?
Covered conditions are conditions that have been approved by the FDA for HBOT. There are currently 13 covered conditions in the U.S. including carbon monoxide poisoning, burns, osteomyelitis, and radiation injuries to name a few. If you fall into any of these categories and would like to try to be reimbursed for HBOT treatment by your insurance provider, please let us how we can help support you with a self-claim.
Non-covered conditions are conditions that have large bodies of research and patient experiences in support of HBOT as an effective therapy. Many of our patients receive treatment for non-covered conditions (also known as “off label” treatment). For a full list of the conditions we treat at Extivita, visit our Conditions page. Additionally, the National Institute of Health (NIH) typically has hundreds of ongoing clinical trials for the use of hyperbaric medicine covering the treatment of conditions such as stroke, cancer, ulcerative colitis, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, chronic fatigue, fibromyalgia, and traumatic brain injuries. For a complete listing, visit the NIH Clinical Trials website.
How many HBOT treatments will I need?
This depends on the condition that you are receiving treatment for, as well as how your body responds to HBOT. The antioxidant and anti-inflammatory effects of HBOT can typically be felt within the first few sessions.
Some post-COVID Long Haulers or patients who are using HBOT within days of a head injury for concussion healing can feel the positive results in as little as 3-5 treatments. Benefits for acute injuries and soft-tissue damage can typically be seen in 5-10 sessions, while chronic injuries typically require 10-20 sessions. Many conditions require 20-40 HBOT sessions for full healing effects such as stem cell increase. During your consult, Elena Schertz will provide you with a suggested HBOT dive schedule to help you achieve optimal healing.
Are there any side-effects to HBOT?
HBOT is generally considered one of the safest therapies in use today. Any serious side effects can be prevented by pre-HBOT screening that all patients receive during their consultation. One side effect that is some people experience is mild ear pain while the chamber pressurizes. However, this can be reduced through proper sinus clearing and it typically goes away as you receive more treatments.
Recent Hyperbaric Oxygen Therapy News & Research
Anti-Aging with Hyperbaric Oxygen Therapy
As we age, many seek ways to maintain vitality, slow the aging process, and boost overall health. One promising approach gaining attention is Hyperbaric Oxygen Therapy (HBOT), which involves breathing 100% oxygen in a pressurized chamber. Not only...
Post-COVID Recovery: Healing with HBOT
Post-COVID challenges can leave many grappling with unresolved health issues. Hyperbaric Oxygen Therapy (HBOT) is a medical treatment that enhances the body's natural healing process by delivering oxygen at higher-than-atmospheric pressures....
Knee Recovery: The Emergence of HBOT as a Game-Changer
Knee injuries, a common plight affecting many from athletes to the elderly, have traditionally been addressed through conventional medical treatments. However, the advent of Hyperbaric Oxygen Therapy (HBOT) is transforming the landscape of knee...
References:
- Bitterman, Haim. “Bench-to-Bedside Review: Oxygen as a Drug.” Critical Care, vol. 13, no. 1, 2009, p. 205. DOI.org (Crossref), doi:10.1186/cc7151.
- Thom, Stephen R., et al. “Stem Cell Mobilization by Hyperbaric Oxygen.” American Journal of Physiology-Heart and Circulatory Physiology, vol. 290, no. 4, Apr. 2006, pp. H1378–86. physiology.org (Atypon), doi:10.1152/ajpheart.00888.2005.
- Thom, Stephen R. “Oxidative Stress Is Fundamental to Hyperbaric Oxygen Therapy.” Journal of Applied Physiology, vol. 106, no. 3, American Physiological Society, Mar. 2009, pp. 988–95. journals.physiology.org (Atypon), doi:10.1152/japplphysiol.91004.2008.
- Godman, Cassandra A., et al. “Hyperbaric Oxygen Treatment Induces Antioxidant Gene Expression.” Annals of the New York Academy of Sciences, vol. 1197, June 2010, pp. 178–83. PubMed, doi:10.1111/j.1749-6632.2009.05393.x.
- Thom, Stephen R. “Hyperbaric Oxygen – Its Mechanisms and Efficacy.” Plastic and Reconstructive Surgery, vol. 127, no. Suppl 1, Jan. 2011, pp. 131S-141S. PubMed Central, doi:10.1097/PRS.0b013e3181fbe2bf.
- Thackham, Jennifer A., et al. “The Use of Hyperbaric Oxygen Therapy to Treat Chronic Wounds: A Review.” Wound Repair and Regeneration, vol. 16, no. 3, 2008, pp. 321–30. Wiley Online Library, doi:10.1111/j.1524-475X.2008.00372.x
- Thom, Stephen R., et al. “Stem Cell Mobilization by Hyperbaric Oxygen.” American Journal of Physiology-Heart and Circulatory Physiology, vol. 290, no. 4, Apr. 2006, pp. H1378–86. physiology.org (Atypon), doi:10.1152/ajpheart.00888.2005.
- Thom, Stephen R., et al. “Stimulation of Perivascular Nitric Oxide Synthesis by Oxygen.” American Journal of Physiology-Heart and Circulatory Physiology, vol. 284, no. 4, Apr. 2003, pp. H1230–39. physiology.org (Atypon), doi:10.1152/ajpheart.01043.2002.
- Aicher, Alexandra, et al. “Essential Role of Endothelial Nitric Oxide Synthase for Mobilization of Stem and Progenitor Cells.” Nature Medicine, vol. 9, no. 11, Nov. 2003, pp. 1370–76. PubMed, doi:10.1038/nm948.
- “CD34+AC133+ Cells Isolated from Cord Blood Are Highly Enriched in Long-Term Culture-Initiating Cells, NOD/SCID-Repopulating Cells and Dendritic Cel… – PubMed – NCBI.” Accessed August 19, 2019. https://www.ncbi.nlm.nih.gov/pubmed/9831864?dopt=Abstract.
- Jiang, Yuehua, Balkrishna N. Jahagirdar, R. Lee Reinhardt, Robert E. Schwartz, C. Dirk Keene, Xilma R. Ortiz-Gonzalez, Morayma Reyes, et al. “Pluripotency of Mesenchymal Stem Cells Derived from Adult Marrow.” Nature 418, no. 6893 (July 4, 2002): 41–49. https://doi.org/10.1038/nature00870.
- Benson, R. M., et al. “Hyperbaric Oxygen Inhibits Stimulus-Induced Proinflammatory Cytokine Synthesis by Human Blood-Derived Monocyte-Macrophages.” Clinical and Experimental Immunology, vol. 134, no. 1, Oct. 2003, pp. 57–62. PubMed Central, doi:10.1046/j.1365-2249.2003.02248.x.
- Thom, Stephen R. “Hyperbaric Oxygen – Its Mechanisms and Efficacy.” Plastic and Reconstructive Surgery, vol. 127, no. Suppl 1, Jan. 2011, pp. 131S-141S. PubMed Central, doi:10.1097/PRS.0b013e3181fbe2bf.
- Godman, Cassandra A., et al. “Hyperbaric Oxygen Treatment Induces Antioxidant Gene Expression.” Annals of the New York Academy of Sciences, vol. 1197, June 2010, pp. 178–83. PubMed, doi:10.1111/j.1749-6632.2009.05393.x.
- Memar, Mohammad Yousef, et al. “Hyperbaric Oxygen Therapy: Antimicrobial Mechanisms and Clinical Application for Infections.” Biomedicine & Pharmacotherapy, vol. 109, Jan. 2019, pp. 440–47. ScienceDirect, doi:10.1016/j.biopha.2018.10.142.
- Çimşit, Maide, et al. “Hyperbaric Oxygen Therapy as an Anti-Infective Agent.” Expert Review of Anti-Infective Therapy, vol. 7, no. 8, Taylor & Francis, Oct. 2009, pp. 1015–26. Taylor and Francis+NEJM, doi:10.1586/eri.09.76.
- Turhan, Vedat, et al. “Hyperbaric Oxygen as Adjunctive Therapy in Experimental Mediastinitis.” Journal of Surgical Research, vol. 155, no. 1, July 2009, pp. 111–15. ScienceDirect, doi:10.1016/j.jss.2008.08.031.
- Lerche, C. J., et al. “Hyperbaric Oxygen Therapy Augments Tobramycin Efficacy in Experimental Staphylococcus Aureus Endocarditis.” International Journal of Antimicrobial Agents, vol. 50, no. 3, Sept. 2017, pp. 406–12. ScienceDirect, doi:10.1016/j.ijantimicag.2017.04.025.