Crohn’s Disease (CD)
Crohn’s Disease is an inflammatory bowel disease (IBD) characterized by chronic inflammation of the gastrointestinal (GI) tract at any location or layer. Patients with Crohn’s typically experience diarrhea, fever, fatigue, abdominal pain, and appetite and weight loss to name the main symptoms(1). More recent findings show that patients with Crohn’s also suffer from mild cognitive impairment(2). The physical symptoms can have a slow onset, a rapid onset, and in some cases, may not appear for long periods of time (remission)(3).
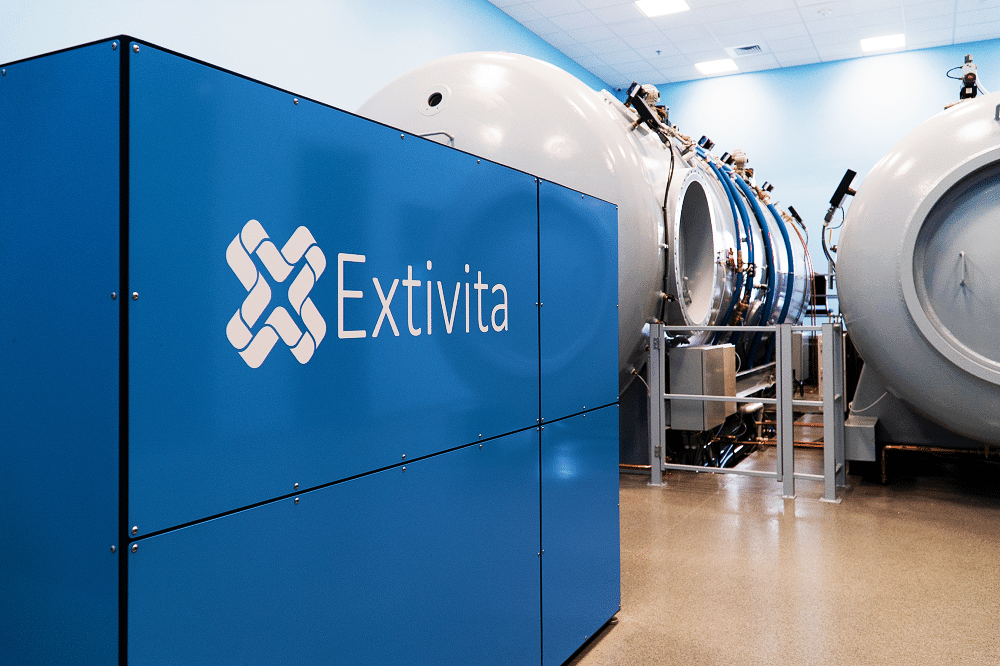
Extivita Therapies for Crohn’s Disease:
Extivita Therapies for Crohn’s Disease Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Hyperbaric Oxygen Therapy for Crohn’s Disease:
A review of research on HBOT and IBD found that 78% of Crohn’s patients experienced significant improvement (complete or partial recovery) when treated with HBOT at 2.0-2.8 ATA(4). The improvements are mainly attributed to HBOT’s proven anti-inflammatory effects(4,5).
More specifically, HBOT has repeatedly been shown to decrease the levels of pro-inflammatory cytokines that are implicated in Crohn’s disease(6). Apart from decreasing inflammation, studies suggest that stem cell therapy has the potential to help heal damaged tissue in Crohn’s patients, and HBOT is known to increase the availability and differentiation of stem cells(7,8,9).
Effects of HBOT on Crohn’s Disease:

Decreased Inflammation
Increased Stem Cell Activity
New Blood Vessel Formation
Hyperbaric oxygen therapy stimulates the formation of new blood vessels, healing injured tissues that were unable to get nutrients and oxygen.

Neurofeedback for Crohn’s Disease:
Research has shown that patient’s with Crohn’s disease very often suffer from cognitive impairment. Compared to healthy individuals, Crohn’s patients exhibit slower information processing speed, higher depression ratings, difficulties sleeping, and fatigue(2). These issues should not be overlooked in the treatment of Crohn’s due to their increasing the likelihood of workplace accidents as well as their potential impact on the patient’s mental health(10). Neurofeedback has been shown to increase processing speed as well as decrease depression ratings, suggesting its potential use for treating patients with Crohn’s disease(11,12).
IV Therapy for Crohn’s Disease:
Studies show that individuals with IBD have lower circulating levels of total antioxidants in their blood during both the active and asymptomatic stages of disease(13). Inflammation from reactive oxygen and nitrogen species, coupled with depletion of antioxidants, contribute to damage of the intestinal walls in patients with IBD. The Myer’s cocktail provides higher serum levels of antioxidants (compared with oral supplementation) which can decrease inflammation, especially that in IBD. When given with glutathione, the Myer’s cocktail can have a powerful synergistic effect on decreasing inflammation and improving the body’s response to stress.


Pulsed Electromagnetic Field Therapy for Crohn’s Disease:
In chronic inflammatory disease like Crohn’s Disease, pulse electromagnetic field (PEMF) therapy can be an effective addition to dietary interventions. PEMF therapy helps by correcting imbalances in the immune system, counteracting inflammatory responses, and supporting healing processes(14, 15).
News & Research for Crohn’s Disease:
Hyperbaric Oxygen Therapy Promising for Crohn’s Fistulas
Hyperbaric oxygen therapy (HBOT) can help heal bowel fistulas in patients with advanced Crohn's disease, according to a systematic review and meta-analysis. Overall, use of HBOT was associated with a 87% clinical response rate...
Investigational HBOT indications: Inflammatory bowel disease
One of the earliest documented cases of HBOT to treat complications of Crohn’s disease (CD) was in 1989. It was a woman with "severe perineal CD that defied medical therapy for eight years". In this particular case the woman was treated with HBOT over a course...
Stem cell-based therapy for inflammatory bowel disease
Abstract Inflammatory bowel disease (IBD) is an idiopathic, multi-etiological disease characterized by inflammation and mucosal destruction of the gastrointestinal tract. Despite the remarkable advance in immunomodulating therapies, there still remains a certain...
References
- “Ulcerative Colitis vs Crohn’s Disease – UCLA Center for Inflammatory Bowel Diseases – Los Angeles, CA.” Accessed July 12, 2019. https://www.crohnsandcolitis.com/ulcerative-colitis?cid=ppc_ppd_ggl_uc_da_colitis_vs_crohn%27s_Phrase_64Z1867746&gclihttps://www.crohnsandcolitis.com/ulcerative-colitis?d=EAIaIQobChMI2faS7anB4wIVCZSzCh1u1wCjEAAYASAAEgI0uvD_BwE
- Langenberg, Daniel R. van, et al. “Cognitive Impairment in Crohn’s Disease Is Associated with Systemic Inflammation, Symptom Burden and Sleep Disturbance:” United European Gastroenterology Journal, SAGE PublicationsSage UK: London, England, Aug. 2016. Sage UK: London, England, journals.sagepub.com, doi:10.1177/2050640616663397.
- “Crohn’s Disease – Symptoms and Causes.” Mayo Clinic. Accessed July 9, 2019. https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304.
- Rossignol, Daniel A. “Hyperbaric Oxygen Treatment for Inflammatory Bowel Disease: A Systematic Review and Analysis.” Medical Gas Research, vol. 2, no. 1, Mar. 2012, p. 6. BioMed Central, doi:10.1186/2045-9912-2-6.
- Thom, Stephen R. “Hyperbaric Oxygen – Its Mechanisms and Efficacy.” Plastic and Reconstructive Surgery, vol. 127, no. Suppl 1, Jan. 2011, pp. 131S-141S. PubMed Central, doi:10.1097/PRS.0b013e3181fbe2bf.
- Papadakis, K. A., and S. R. Targan. “The Role of Chemokines and Chemokine Receptors in Mucosal Inflammation.” Inflammatory Bowel Diseases, vol. 6, no. 4, Nov. 2000, pp. 303–13. PubMed, doi:10.1002/ibd.3780060408.
- Garcia-Olmo, Damian, Mariano Garcia-Arranz, and Dolores Herreros. “Expanded Adipose-Derived Stem Cells for the Treatment of Complex Perianal Fistula Including Crohn’s Disease.” Expert Opinion on Biological Therapy 8, no. 9 (September 2008): 1417–23. https://doi.org/10.1517/14712598.8.9.1417.
- Shimizu, Hiromichi, et al. “Stem Cell-Based Therapy for Inflammatory Bowel Disease.” Intestinal Research, vol. 17, no. 3, July 2019, pp. 311–16. PubMed Central, doi:10.5217/ir.2019.00043.
- Milovanova, Tatyana N., Veena M. Bhopale, Elena M. Sorokina, Jonni S. Moore, Thomas K. Hunt, Martin Hauer-Jensen, Omaida C. Velazquez, and Stephen R. Thom. “Hyperbaric Oxygen Stimulates Vasculogenic Stem Cell Growth and Differentiation in Vivo.” Journal of Applied Physiology 106, no. 2 (February 2009): 711–28. https://doi.org/10.1152/japplphysiol.91054.2008.
- Swaen, G. M. H., et al. “Fatigue as a Risk Factor for Being Injured in an Occupational Accident: Results from the Maastricht Cohort Study.” Occupational and Environmental Medicine, vol. 60, no. suppl 1, BMJ Publishing Group Ltd, June 2003, pp. i88–92. oem.bmj.com, doi:10.1136/oem.60.suppl_1.i88.
- Angelakis, Efthymios, et al. “EEG Neurofeedback: A Brief Overview and an Example of Peak Alpha Frequency Training for Cognitive Enhancement in the Elderly.” The Clinical Neuropsychologist, vol. 21, no. 1, Jan. 2007, pp. 110–29. PubMed, doi:10.1080/13854040600744839.
- Choi, Sung Won, et al. “Is Alpha Wave Neurofeedback Effective with Randomized Clinical Trials in Depression? A Pilot Study.” Neuropsychobiology; Basel, vol. 63, no. 1, S. Karger AG, Nov. 2010, pp. 43–51. ProQuest, doi:http://dx.doi.org.go.libproxy.wakehealth.edu/10.1159/000322290.
- Moura, Fabiana Andréa et al. “Antioxidant therapy for treatment of inflammatory bowel disease: Does it work?.” Redox biology vol. 6 (2015): 617-639. doi:10.1016/j.redox.2015.10.006
- Klopp, Rainer Christian et al. “Effects of various physical treatment methods on arteriolar vasomotion and microhemodynamic functional characteristics in case of deficient regulation of organ blood flow. Results of a placebo-controlled, double-blind study.” Journal of complementary & integrative medicine vol. 10,Suppl (2013): S39-46, S41-9. doi:10.1515/jcim-2013-0035
- Kubat, Nicole J et al. “Effect of pulsed electromagnetic field treatment on programmed resolution of inflammation pathway markers in human cells in culture.” Journal of inflammation research vol. 8 59-69. 23 Feb. 2015, doi:10.2147/JIR.S78631



