Insomnia
High quality sleep is incredibly important. Unfortunately, an estimated 20-30% of adults in the United States suffer from insomnia, and this number is increasing exponentially(1-3). Insomnia refers to trouble falling asleep and/or trouble staying asleep that occurs three or more times a week and can be considered short-term (persists for less than 3 months) or chronic (persists for more than 3 months). Due to its negative impact on normal daily functioning, insomnia is linked to increased risk of physiological diseases including cardiovascular disease, cancer, and diabetes(5). Additionally, many people with neurological issues such as post-traumatic stress disorder, traumatic brain injury, depression, anxiety, and substance abuse(6-12).
Due to its association with so many other disorders, all of which have their own detrimental health effects, the treatment of insomnia is incredibly important. We highly recommend neurofeedback therapy (supported by IV and PEMF therapy) for those who are looking for long-lasting relief of their insomnia, as well as those who have a poor response to conventional therapies.
Extivita Therapies for Insomnia:
Extivita Therapies for Insomnia:

Neurofeedback

IV Therapy
Bemer
Supplements
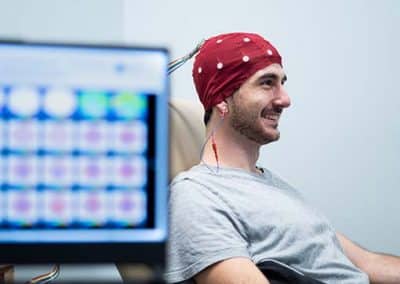
Neurofeedback Therapy for Insomnia:
Neurofeedback can be incredibly successful in improving sleep quality and duration in those with insomnia. Specific protocols typically involve increasing the sensorimotor rhythm (SMR), which refers to activity between 12-15Hz in the central/parietal region of the head. Increasing SMR has been shown to successfully improved insomnia, perhaps because an increase in SMR may lead to increased sleep spindles, which are associated with improved quality and duration of sleep(13-16). Additionally, increasing SMR may improve insomnia by increasing relaxation and decreasing excessive motor activity(17).
Some insomnia protocols may also work to decrease beta and high beta activity (15-30Hz) if elevated, as too much beta activity can indicate a constant state of hyperarousal(14, 18). The specific protocol for someone with insomnia depends on a careful analysis of that individuals qEEG brain map, their behavioral assessment, and their neurofeedback consultation.
Nutritional IV Therapy for Insomnia:
We strongly recommend our Myer’s Cocktail IV and Glutathione IV for those with insomnia due to their antioxidant and nutritional benefits. Insomnia has been associated with increased levels of oxidative stress, something that occurs when 1) there are elevated levels of reactive oxygen species and/or 2) there are deficient antioxidant defenses(19).
Both Vitamin C, which is in the Myer’s Cocktail IV, and Glutathione are powerful antioxidants that scavenges and eliminates damaging free radicals thereby decreasing oxidative stress(20-21). Deficient glutathione levels have also been observed in people with insomnia(19). Additionally, both Magnesium and B Vitamins (components of the Myer’s Cocktail IV) have been shown to improve sleep-related issues(22-24).


Pulsed Electromagnetic Field Therapy for Insomnia:
There is evidence to suggest that pulsed-electromagnetic field therapy (PEMF) may improve sleep duration, sleep quality, and overall insomnia severity in those with insomnia (25-26). One study found that 70% of participants experienced “very clear improvement” or better and 94% reported “clear improvement” after 4 weeks of PEMF therapy(26).
News & Research for Insomnia:
Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy
nsomnia, whether short-term or chronic, is a common condition. It has a negative impact on vulnerable patient groups, including active military personnel and veterans, patients with coexisting psychiatric and medical disorders, those in life transitions such as menopause, and elderly persons. Although cognitive behavioral therapy for insomnia (CBTI) is first-line treatment for insomnia, its high cost and a lack of trained providers has prevented widespread uptake. Now, digital CBTI (dCBTI) is emerging as a scalable option with the potential to overcome these barriers in managed care.
Focusing on insomnia symptoms to better understand depression: A STAR*D report
Abstract Background: Disturbed sleep is a core symptom of major depressive disorder (MDD), with nearly 90% of those with MDD reporting disturbed sleep. However, combining insomnia and hypersomnia into a single diagnostic domain ignores distinct biological differences...
Novel non-pharmacological insomnia treatment – a pilot study
Abstract Objective: The objective of this prospective pilot study was to examine the effects of a novel non-pharmacological device (BioBoosti) on insomnia symptoms in adults. Methods: Subjects with chronic insomnia were instructed to hold the device in each hand for 8...
References
- Roth, Thomas, et al. “Prevalence and Perceived Health Associated with Insomnia Based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition Criteria: Results from the America Insomnia Survey.” Biological Psychiatry, vol. 69, no. 6, Mar. 2011, pp. 592–600. PubMed, doi:10.1016/j.biopsych.2010.10.023.
- Moloney, Mairead Eastin, et al. “The Medicalization of Sleeplessness: Results of U.S. Office Visit Outcomes, 2008-2015.” SSM – Population Health, vol. 8, Aug. 2019, p. 100388. PubMed, doi:10.1016/j.ssmph.2019.100388.
- “Insomnia Overview: Epidemiology, Pathophysiology, Diagnosis and Monitoring, and Nonpharmacologic Therapy.” AJMC, https://www.ajmc.com/view/insomnia-overview-epidemiology-pathophysiology-diagnosis-and-monitoring-and-nonpharmacologic-therapy. Accessed 11 Feb. 2021.
- Insomnia | NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/insomnia. Accessed 11 Feb. 2021.
- Hafner, Marco, et al. “Why Sleep Matters-The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis.” Rand Health Quarterly, vol. 6, no. 4, Jan. 2017, p. 11.
- Hughes, Jaime M., et al. “Insomnia in United States Military Veterans: An Integrated Theoretical Model.” Clinical Psychology Review, vol. 59, Feb. 2018, pp. 118–25. PubMed, doi:10.1016/j.cpr.2017.11.005.
- Wickwire, Emerson M., et al. “Sleep, Sleep Disorders, and Circadian Health Following Mild Traumatic Brain Injury in Adults: Review and Research Agenda.” Journal of Neurotrauma, vol. 35, no. 22, Nov. 2018, pp. 2615–31. PubMed, doi:10.1089/neu.2017.5243.
- Mason, Brittany L., et al. “Focusing on Insomnia Symptoms to Better Understand Depression: A STAR*D Report.” Journal of Affective Disorders, vol. 260, Jan. 2020, pp. 183–86. PubMed, doi:10.1016/j.jad.2019.08.094.
- Ford, D. E., and D. B. Kamerow. “Epidemiologic Study of Sleep Disturbances and Psychiatric Disorders. An Opportunity for Prevention?” JAMA, vol. 262, no. 11, Sept. 1989, pp. 1479–84. PubMed, doi:10.1001/jama.262.11.1479.
- Chakravorty, Subhajit, et al. “Alcohol Dependence and Its Relationship With Insomnia and Other Sleep Disorders.” Alcoholism, Clinical and Experimental Research, vol. 40, no. 11, Nov. 2016, pp. 2271–82. PubMed, doi:10.1111/acer.13217.
- Roehrs, Timothy, and Thomas Roth. “Insomnia as a Path to Alcoholism: Tolerance Development and Dose Escalation.” Sleep, vol. 41, no. 8, May 2018. PubMed Central, doi:10.1093/sleep/zsy091.
- Chakravorty, Subhajit, et al. “Sleep Management Among Patients with Substance Use Disorders.” The Medical Clinics of North America, vol. 102, no. 4, July 2018, pp. 733–43. PubMed, doi:10.1016/j.mcna.2018.02.012.
- Hammer, Barbara U., et al. “Neurofeedback for Insomnia: A Pilot Study of Z-Score SMR and Individualized Protocols.” Applied Psychophysiology and Biofeedback, vol. 36, no. 4, Dec. 2011, pp. 251–64. PubMed, doi:10.1007/s10484-011-9165-y.
- Cortoos, Aisha, et al. “An Exploratory Study on the Effects of Tele-Neurofeedback and Tele-Biofeedback on Objective and Subjective Sleep in Patients with Primary Insomnia.” Applied Psychophysiology and Biofeedback, vol. 35, no. 2, June 2010, pp. 125–34. DOI.org (Crossref), doi:10.1007/s10484-009-9116-z.
- Schabus, Manuel, et al. “Better than Sham? A Double-Blind Placebo-Controlled Neurofeedback Study in Primary Insomnia.” Brain, vol. 140, no. 4, Apr. 2017, pp. 1041–52. Silverchair, doi:10.1093/brain/awx011.
- Andrillon, Thomas, et al. “Sleep Spindles in Humans: Insights from Intracranial EEG and Unit Recordings.” The Journal of Neuroscience, vol. 31, no. 49, Dec. 2011, pp. 17821–34. PubMed Central, doi:10.1523/JNEUROSCI.2604-11.2011.
- Sterman, M. Barry. “Basic Concepts and Clinical Findings in the Treatment of Seizure Disorders with EEG Operant Conditioning.” Clinical Electroencephalography, vol. 31, no. 1, SAGE Publications, Jan. 2000, pp. 45–55. SAGE Journals, doi:10.1177/155005940003100111.
- Perlis, Michael L., et al. “Beta/Gamma EEG Activity in Patients with Primary and Secondary Insomnia and Good Sleeper Controls.” Sleep, vol. 24, no. 1, Jan. 2001, pp. 110–17. Silverchair, doi:10.1093/sleep/24.1.110.
- Gulec, Mustafa, et al. “Oxidative Stress in Patients with Primary Insomnia.” Progress in Neuro-Psychopharmacology and Biological Psychiatry, vol. 37, no. 2, June 2012, pp. 247–51. ScienceDirect, doi:10.1016/j.pnpbp.2012.02.011.
- Traber, Maret G., and Jan F. Stevens. “Vitamins C and E: Beneficial Effects from a Mechanistic Perspective.” Free Radical Biology & Medicine, vol. 51, no. 5, Sept. 2011, pp. 1000–13. PubMed Central, doi:10.1016/j.freeradbiomed.2011.05.017.
- Forman, Henry Jay, et al. “Glutathione: Overview of Its Protective Roles, Measurement, and Biosynthesis.” Molecular Aspects of Medicine, vol. 30, no. 1–2, 2009, pp. 1–12. PubMed Central, doi:10.1016/j.mam.2008.08.006.
- Abbasi, Behnood, et al. “The Effect of Magnesium Supplementation on Primary Insomnia in Elderly: A Double-Blind Placebo-Controlled Clinical Trial.” Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, vol. 17, no. 12, Dec. 2012, pp. 1161–69.
- Djokic, Gorica, et al. “The Effects of Magnesium – Melatonin – Vit B Complex Supplementation in Treatment of Insomnia.” Open Access Macedonian Journal of Medical Sciences, vol. 7, no. 18, Aug. 2019, pp. 3101–05. PubMed Central, doi:10.3889/oamjms.2019.771.
- Lothian, Joanna, et al. “Effect of Micronutrients on Insomnia in Adults: A Multiple-Baseline Study.” Clinical Psychological Science, vol. 4, no. 6, SAGE Publications Inc, Nov. 2016, pp. 1112–24. SAGE Journals, doi:10.1177/2167702616631740.
- Pavlova, Milena K., et al. “Novel Non-Pharmacological Insomnia Treatment – a Pilot Study.” Nature and Science of Sleep, vol. 11, Sept. 2019, pp. 189–95. PubMed Central, doi:10.2147/NSS.S198944.
- Pelka, R. B., et al. “Impulse Magnetic-Field Therapy for Insomnia: A Double-Blind, Placebo-Controlled Study.” Advances in Therapy, vol. 18, no. 4, Aug. 2001, pp. 174–80. PubMed, doi:10.1007/BF02850111.