Surgery
Surgery is a medical procedure where an opening into the body is performed through small or large incisions to treat or manage injuries and diseases. Types of surgeries range from simple dental procedures to complicated brain surgeries. All surgery results in an incision or wound, which produces a natural inflammatory response to promote healing. Even a seemingly harmless surgical intervention can overwhelm the immune system, which can lead to suboptimal wound healing and/or post operative complications(1).
Extivita Therapies for Surgical Patients:
Extivita Therapies for Surgical Patients:
Hyperbaric Oxygen Therapy

Nutritional IV Therapy
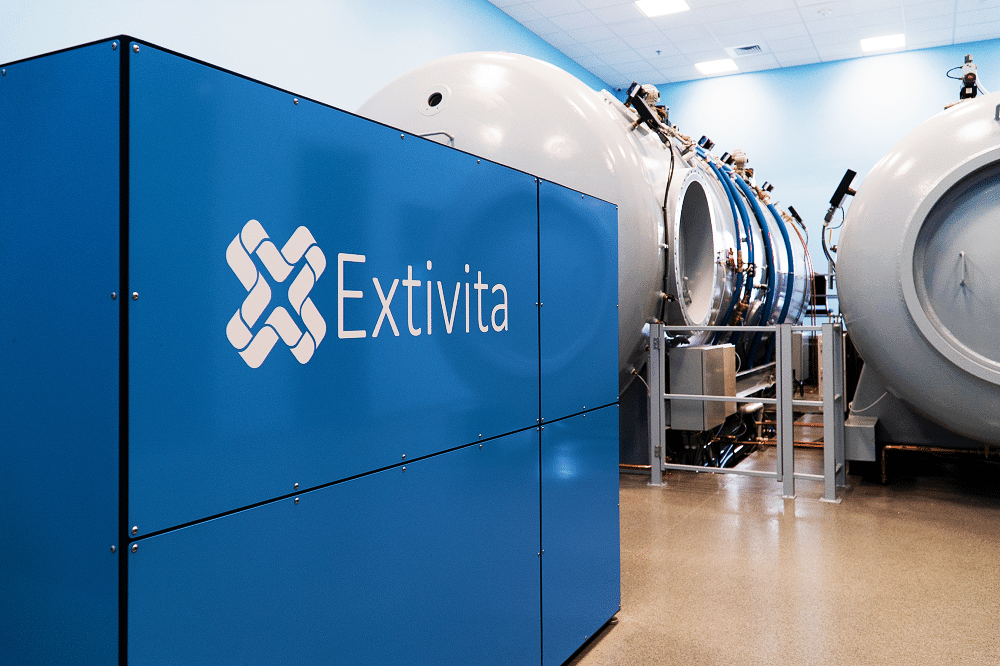
What is HBOT?
Hyperbaric Oxygen Therapy, or “HBOT,” involves breathing 100% oxygen in a pressurized chamber to significantly increase oxygen supply to your cells and tissues. HBOT has such a large therapeutic range because of the positive changes it induces on several key systems; especially the circulatory, immune, and regenerative systems.
HBOT Research Shows How Surgical Patients May Benefit:
HBOT is an effective treatment for surgery, both pre-operatively and post-operatively. Pre-operative benefits include increased antioxidant production, which helps protect cells from oxidative damage and inflammation (1). It has also been shown to increase ischemic tolerance, induce neuroprotection, and decrease post-surgical complications (1,2,3). Research shows that there is a link between cognitive decline, surgery, and anesthesia. HBOT can prevent cognitive impairment after surgery(1).
HBOT can also accelerate recovery and be an effective adjuvant therapy for addressing surgical wounds that are not healing properly (4).
Effects of HBOT on Surgical Patients:

Decreased Inflammation
New Blood Vessel Formation
Increased Stem Cell Activity
Hyperbaric oxygen therapy mobilizes stem progenitor cells (SPCs) from the bone marrow, creating the opportunity for tissue regeneration.

Antibacterial & Antimicrobial
Hyperbaric oxygen therapy has been shown to target infections and harmful bacteria, both directly and as a supplement to conventional antibiotics.
HBOT for Plastic Surgery or Cosmetic Procedures:
Patients who undergo plastic surgery or aesthetic/cosmetic procedures may greatly benefit from HBOT to help heal faster and avoid surgical complications. Research has shown favorable results when HBOT is used in the treatment of wounds, inflammation, and infection(3-5). A significant increase in oxygen in the blood (up to 800% more than what we are normally breathing) and subsequently the tissues, has many positive effects; including decreased pain, redness, bruising, and swelling. HBOT also helps fight infections and increases collagen formation.
In patients who received hair transplantation surgery, HBOT minimized pain, follicle shedding, itchiness, and folliculitis(6) . HBOT has been shown to enhance and expedite the healing process, shorten recovery time from procedures like facelifts, hair transplants, liposuction, breast augmentation and more.

IV Therapy for Surgical Patients:
Why Use IV Therapy?
When nutrients are given intravenously (through an IV), nearly 100% of those nutrients are available to your tissues and cells via your bloodstream. This allows for optimal absorption, something that is not attainable with oral supplements due to the loss during digestion. IVs also get nutrients to your tissues at a much quicker rate than other forms of nutrient supplementation. This combination of quick and maximum absorption makes IV therapy one of the most effective ways to combat nutrient deficiencies and imbalances in your body.
Quickest, most effective way to supply your cells with the nutrients they need

Customized nutrient add-ons to target your specific health concerns
Detoxifies, boosts energy, relieves stress, and so much more
IV Therapy Research Shows How Surgical Patients May Benefit:
Intravenous Vitamin C in our Myer’s cocktail produces many positive effects pre- and post-surgery. It is an essential nutrient which plays a major role in all phases of wound healing, functioning as both cofactor and potent antioxidant(8). As a cofactor, Vitamin C promotes collagen formation, important in tissue repair and regeneration. As an antioxidant, Vitamin C removes toxins, is anti-microbial, and contributes to immune defense making it both anti-inflammatory and cell protective(9). Studies have shown that Vitamin C levels decrease after surgery(10). Such a deficiency can impair wound healing, immunity, and lead to higher susceptibility to infection, resulting in further inflammation and pain.


Pulsed Electromagnetic Field Therapy (PEMF) for Surgical Patients:
Pulsed electromagnetic field therapy significantly reduces both acute and chronic post-operative pain, inflammation, and narcotic use (10-11). PEMF signals modulate anti-inflammatory pathways, decreasing inflammatory cytokines such as IL-1 B, effecting nitric oxide signaling, leading to faster, higher quality surgical wound repair (12).
What is Pulsed Electromagnetic Field Therapy (PEMF)?
There are many pulsed electromagnetic field (PEMF) generators in the market, all of which use different signal formats producing different effects. Extivita uses the BEMER, which stands for Bio-Electro-Magnetic-Energy-Regulation BEMER is an FDA Class II cleared consumer medical device that is non-invasive.
The BEMER uses PEMF to deliver a patented bio-rhythmically defined therapeutic signal which temporarily increases local blood flow (micro circulation). The device does this by delivering safe, electromagnetic fields with various organized waveforms that facilitate optimal health. The safety of PEMF devices is supported by thousands of clinical trials and scientific studies.
What is Infared Sauna?
You’re probably familiar with traditional saunas if you’ve ever been to a spa or wellness retreat. While traditional saunas can have great stress-relieving benefits, infrared saunas are another type of sauna that can make an even greater impact on your health. Unlike a traditional steam sauna, infrared saunas use light to generate heat which only warms your body and not the air around you.
At Extivita, we use a state-of-the-art full spectrum infrared sauna boasting the lowest and safest EMF and ELF levers of any infrared sauna on the market. While many saunas only use far-infrared wavelengths, ours delivers near-infrared (IR-A), mid-infrared (IR-B) and far-infrared (IR-C) light. Additionally, our sauna delivers over 25 times the power of the nearest clinics’, allowing for the deepest tissue penetration and optimal health benefits.

Incredibly relaxing, safe therapy with few common side effects
State of the art, full-spectrum infrared sauna
Helps improve circulation, decrease inflammation, detoxify, and more!
Infrared Sauna for Surgical Patients:
The biological effects of Far infrared rays have shown to have an effect that promotes wound healing. Studies show that FIR decreases inflammatory cytokines, induces collagen and fibroblasts proliferation, improves mitochondrial function, and mediates other genes to assist in skin wound healing (13-14).

News & Research for Surgery:
Plastic Surgery Patients Heal Faster With HBOT
How does HBOT work? Hyperbaric oxygen therapy, works by exposing the body to an atmosphere of 100% oxygen while inside a pressurized chamber. HBOT helps to reduce swelling and discomfort while providing your body with at least 10–15 times its normal supply of oxygen....
“I Have a Chance to Survive”: 58-Year-Old Ronnie Coleman, Who Has Gone Through 13 Surgeries, Fights Through His Medical Obstacles
Legendary bodybuilder Ronnie Coleman is often called ‘The King’ of modern bodybuilding. Establishing unbelievable dominance, the champion bodybuilder won the Mr. Olympia title for eight years consecutively. Coleman was injured multiple times during his career. He...
This Relaxing 90-Minute Treatment Can Speed Your Healing Post-Plastic Surgery
Plastic surgery is no walk in the park, but the real challenge begins once you wake up and begin to heal. After popular procedures like rhinoplasties, breast augmentations, or facelifts, you will not exactly want to get up and dance on the table. While sedated or...
References
- Gao, Zhi-Xin et al. “Hyperbaric oxygen preconditioning improves postoperative cognitive dysfunction by reducing oxidant stress and inflammation.” Neural regeneration research vol. 12,2 (2017): 329-336. doi:10.4103/1673-5374.200816
- Alex, Joseph et al. “Pretreatment with hyperbaric oxygen and its effect on neuropsychometric dysfunction and systemic inflammatory response after cardiopulmonary bypass: a prospective randomized double-blind trial.” The Journal of thoracic and cardiovascular surgery vol. 130,6 (2005): 1623-30. doi:10.1016/j.jtcvs.2005.08.018
- Friedman, Tali et al. “Hyperbaric Oxygen Preconditioning Can Reduce Postabdominoplasty Complications: A Retrospective Cohort Study.” Plastic and reconstructive surgery. Global open vol. 7,10 e2417. 31 Oct. 2019, doi:10.1097/GOX.0000000000002417
- Lopes, André et al. “Hyperbaric oxygen therapy as adjuvant for treating wound complications after extensive resection for vulvar malignancy.” Undersea & hyperbaric medicine : journal of the Undersea and Hyperbaric Medical Society, Inc vol. 45,1 (2018): 27-32.
- Bassetto, Franco et al. “Hyperbaric oxygen therapy in Plastic Surgery practice: case series and literature overview.” Il Giornale di chirurgia vol. 40,4 (2019): 257-275.
- Fan, Zhe-Xiang et al. “The effect of hyperbaric oxygen therapy combined with hair transplantation surgery for the treatment of alopecia.” Journal of cosmetic dermatology vol. 20,3 (2021): 917-921. doi:10.1111/jocd.13665
- Moores, Jane. “Vitamin C: a wound healing perspective.” British journal of community nursing vol. Suppl (2013): S6, S8-11. doi:10.12968/bjcn.2013.18.sup12.s6
- Carr, Anitra C, and Silvia Maggini. “Vitamin C and Immune Function.” Nutrients vol. 9,11 1211. 3 Nov. 2017, doi:10.3390/nu9111211
- Hill, Aileen et al. “Perioperative Vitamin C and E levels in Cardiac Surgery Patients and Their Clinical Significance.” Nutrients vol. 11,9 2157. 9 Sep. 2019, doi:10.3390/nu11092157
- Khooshideh, Maryam et al. “Pulsed Electromagnetic Fields for Postsurgical Pain Management in Women Undergoing Cesarean Section: A Randomized, Double-Blind, Placebo-controlled Trial.” The Clinical journal of pain vol. 33,2 (2017): 142-147. doi:10.1097/AJP.0000000000000376
- Sorrell, Robert Gordon et al. “Evaluation of pulsed electromagnetic field therapy for the treatment of chronic postoperative pain following lumbar surgery: a pilot, double-blind, randomized, sham-controlled clinical trial.” Journal of pain research vol. 11 1209-1222. 22 Jun. 2018, doi:10.2147/JPR.S164303
- Rohde, Christine et al. “Effects of pulsed electromagnetic fields on interleukin-1 beta and postoperative pain: a double-blind, placebo-controlled, pilot study in breast reduction patients.” Plastic and reconstructive surgery vol. 125,6 (2010): 1620-1629. doi:10.1097/PRS.0b013e3181c9f6d3
- Hsu, YH., Chen, YW., Cheng, CY. et al. Detecting the limits of the biological effects of far-infrared radiation on epithelial cells. Sci Rep 9, 11586 (2019). https://doi.org/10.1038/s41598-019-48187-0
- Hsu, Yung-Ho et al. “Far infrared promotes wound healing through activation of Notch1 signaling.” Journal of molecular medicine (Berlin, Germany) vol. 95,11 (2017): 1203-1213. doi:10.1007/s00109-017-1580-y