Hyperbaric Oxygen Therapy helps heal a severe traumatic brain injury in India! Not all hopes die if you know the way out and believe in miracles. When 36-year-old Mr. Pravin Raj Radha met with a fatal accident in the US after he fell from his bicycle in May 2022, he...
Traumatic Brain Injury (TBI)
Hyperbaric Oxygen Therapy (HBOT) Research for Traumatic Brain Injury (TBI).
A Case Series of 39 United States Veterans with Mild Traumatic Brain Injury Treated with Hyperbaric Oxygen Therapy
Abstract: Importance: The Defense and Veterans Brain Injury Center reported 358,088 mild traumatic brain injury (mTBI) among U.S. service members worldwide between the years 2000 and 2020. Veterans with mTBI have higher rates of Post-Traumatic Stress Disorder (PTSD),...
Can Hyperbaric Oxygen Heal Your Brain?
Research supports hyperbaric oxygen therapy as a treatment for mild brain injuries and Alzheimers disease, but it remains controversial as a treatment for autism.(Nakleyka/Shuttertock) A new study shows promising results for this alternative treatment BY JENNIFER...
Systematic Review and Dosage Analysis: Hyperbaric Oxygen Therapy Efficacy in Mild Traumatic Brain Injury Persistent Postconcussion Syndrome
Background: Mild traumatic brain injury results in over 15% of patients progressing to Persistent Postconcussion Syndrome, a condition with significant consequences and limited treatment options. Hyperbaric oxygen therapy has been applied to Persistent...
Hyperbaric oxygen therapy for mild traumatic brain injury persistent postconcussion syndrome: a randomized controlled trial
Abstract: Persistent postconcussion syndrome (PPCS) after mild traumatic brain injury (mTBI) is a significant public health and military problem for which there is limited treatment evidence. The aim of this study was to determine whether forty 150 kPa hyperbaric...
The role of pulsed magnetic fields in the management of concussion and traumatic brain injury
Abstract Traumatic brain injury (TBI) is a complex clinical phenomenon. (Raji) The classic designations of mild, moderate, or severe TBI are based on the acute clinical presentation and do not necessarily predict the long-term outcome. The long held assumption that...
Treatment of Traumatic Brain Injury With Hyperbaric Oxygen Therapy
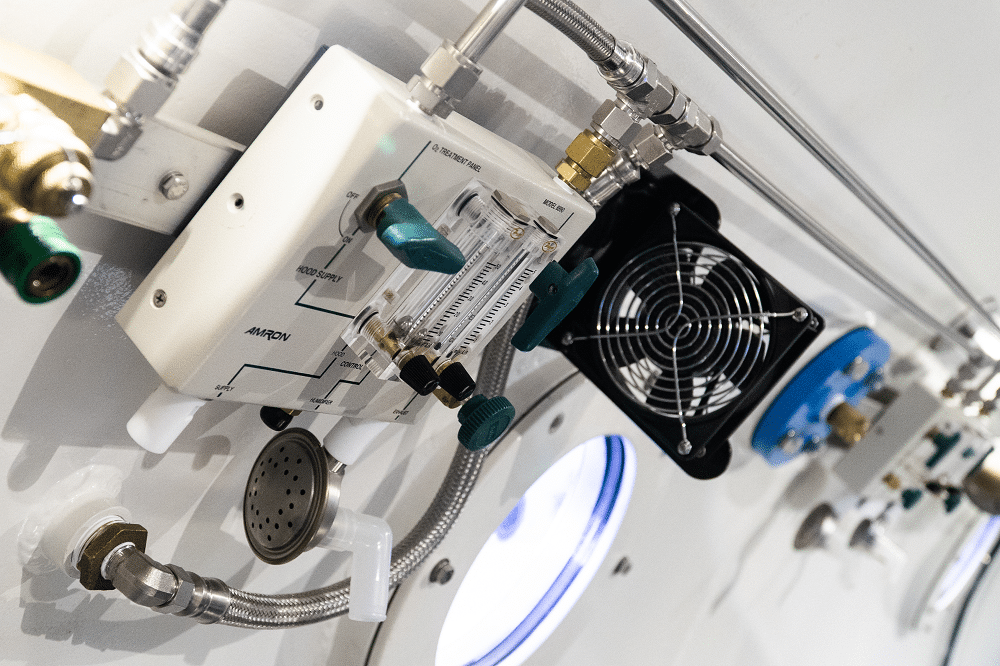
Hyperbaric oxygen therapy (HBOT) is defined as the use of oxygen at higher than atmospheric pressure for the treatment of underlying disease processes and the diseases they produce. Modern HBOT in which 100% O2 is breathed in a pressurized chamber dates back to the 1930s, when it was first used for treatment of decompression illness in divers. There are currently 13 FDA-approved uses for HBOT, including decompression illness, gas gangrene, air embolism, osteomyelitis, radiation necrosis, and the most recent addition—diabetic ulcers. HBOT can dramatically and permanently improve symptoms of chronic TBI months or even many years after the original head injury. This assertion is generally met with skepticism within the medical establishment because we have been taught for generations that any post-concussion symptoms persisting more than 6 months or so after a head injury are due to permanent brain damage that cannot be repaired.
The National Brain Injury Rescue and Rehabilitation Study – a multicenter observational study of hyperbaric oxygen for mild traumatic brain injury with post-concussive symptoms
The National Brain Injury Rescue and Rehabilitation Project was established as a preliminary study to test the safety and practicality of multi-center hyperbaric oxygen administration for the post-concussive symptoms of chronic mild traumatic brain injury as a precursor to a pivotal, independent, multi-center, controlled clinical trial. This report presents the results for 32 subjects who completed a preliminary trial of hyperbaric oxygen several years before the passage of the 21 st Century Cures Act. This study anticipated the Act and its reassessment of clinical research. Subjects received 40-82 one-hour treatments at 1.5 atmospheres absolute 100% oxygen. Outcome measures included repeated self-assessment measures and automated neurocognitive tests. The subjects demonstrated improvement in 21 of 25 neurocognitive test measures observed. The objective neurocognitive test components showed improvement in 13 of 17 measures. Earlier administration of hyperbaric oxygen post injury, younger age at the time of injury and hyperbaric oxygen administration, military status, and increased number of hyperbaric oxygen administrations were characteristics associated with improved outcomes. There were no adverse events. Hyperbaric oxygen was found to be safe, inexpensive and worthy of clinical application in the 21 st Century model of facile data collection provided by recent research regulatory shifts in medicine. The study was approved by the ethics review committee of the Western Institutional Review Board (WIRB; Protocol #20090761).
Textbook of Traumatic Brain Injury
Despite the increased public awareness of traumatic brain injury (TBI), the complexities of the neuropsychiatric, neuropsychological, neurological, and other physical consequences of TBI of all severities across the lifespan remain incompletely understood by patients,...