Neurofeedback
Train Your Brain to Work Better—Naturally
Non-invasive, drug-free neurofeedback therapy to improve cognitive performance, emotional regulation, and neurological balance.
Neurofeedback, also called EEG biofeedback, helps your brain shift into healthier activity patterns by using real-time feedback based on your brainwave data. This therapy is commonly used to help improve attention, reduce reactivity to stress, and enhance emotional regulation.
Explore in-clinic or home-based neurofeedback options tailored to your brain’s unique needs.
Quick Overview: What is Neurofeedback?
Neurofeedback is a non-invasive, drug-free therapy that uses real-time feedback from your brainwave activity (EEG) to help your brain regulate itself more effectively. By encouraging optimal patterns of brain activity, neurofeedback supports improved focus, emotional balance, sleep, and cognitive performance.
At Extivita, we use advanced brain mapping (QEEG) and personalized protocols to guide your training experience. Whether your goals involve better mental clarity, reduced stress, or neurological support, neurofeedback can help your brain perform at its best.
Disclaimer: Neurofeedback is FDA-cleared for general relaxation and stress reduction. Its use for specific conditions is considered investigational and off-label. Individual results may vary.
Request More Information
Take a Deeper Dive (Expands Section) →
Deep Dive: How Neurofeedback Trains the Brain
Neurofeedback is a powerful self-regulation training technique that teaches your brain how to function at its best. Using real-time feedback from brainwave activity, it rewards the brain when it shifts into more balanced and optimal states. Over time, this encourages healthier patterns that support emotional regulation, focus, sleep, and cognitive performance.
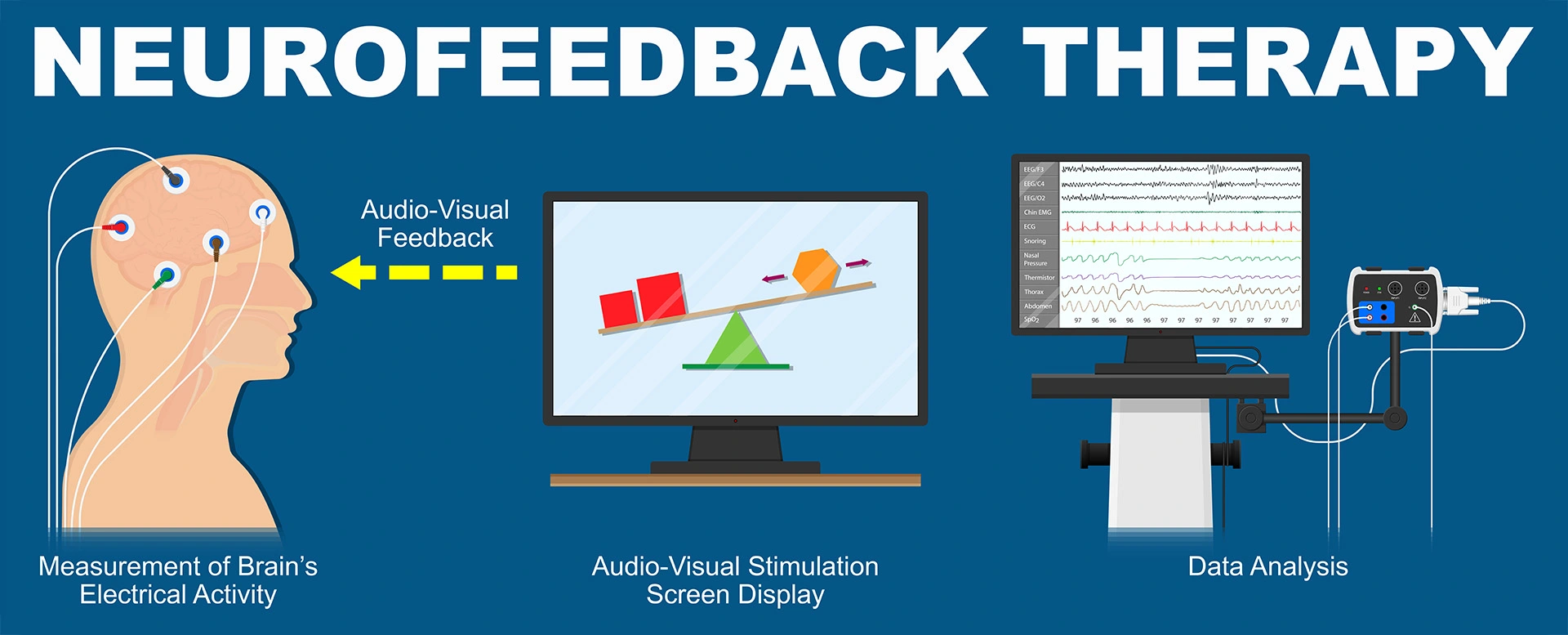
How Feedback Works
During a session, sensors are placed on your scalp to read brainwave activity. As you interact with a visual (such as a video or game) and audio environment, your brain receives immediate cues when it’s operating in the desired range.
This is called operant conditioning, and it helps your brain “learn” the reward of being in a calm, focused, or regulated state.
Visual Cues
Audio Cues
Brain Plasticity in Action
This process takes advantage of neuroplasticity, the brain’s natural ability to rewire itself based on experience. With repeated feedback over multiple sessions, your brain builds new pathways that make those healthier states more accessible—even outside of training.

Understanding Your Brainwaves
Each brainwave frequency is linked to specific mental states. Here are the key ones targeted in neurofeedback:
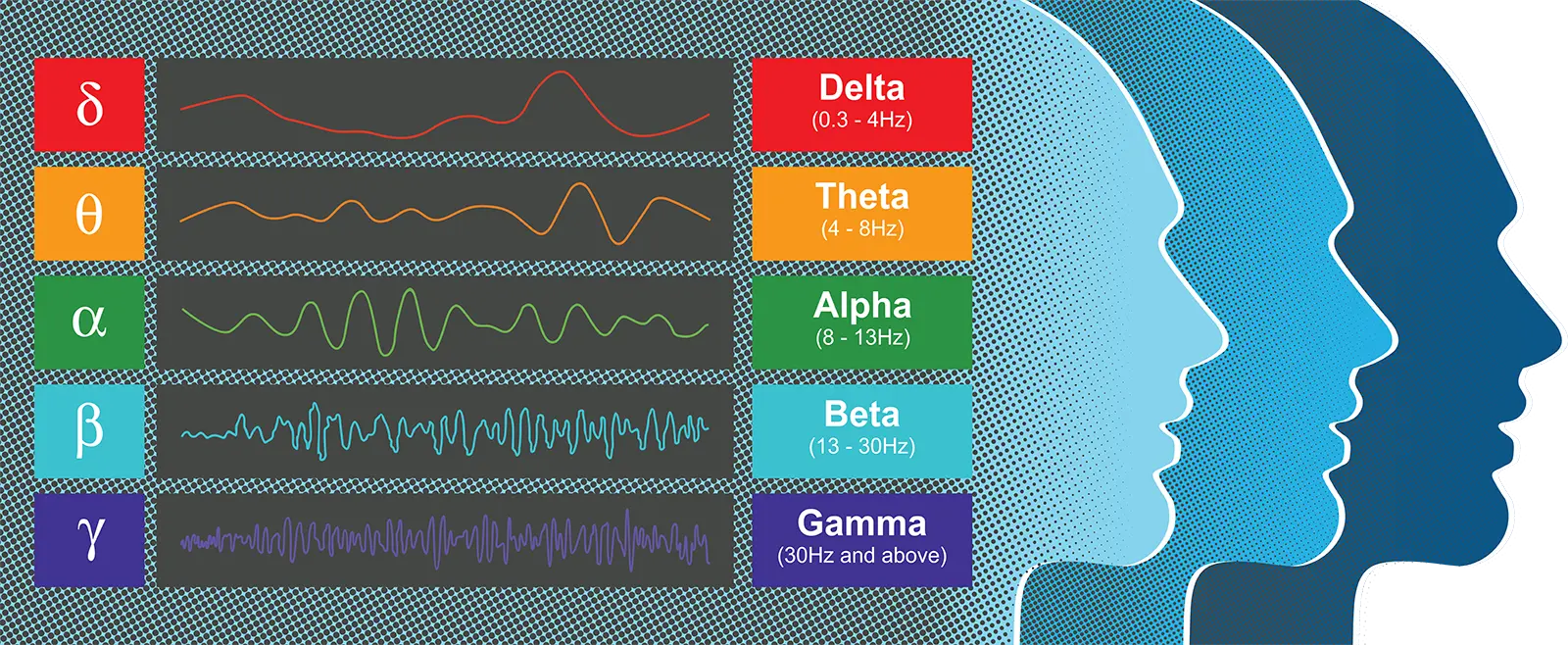
Delta (0.5–4 Hz) – Deep Rest and Healing
Supports deep sleep and physical recovery. Excess delta during waking hours may impair cognition.
Theta (4–8 Hz) – Emotion and Creativity
Linked to daydreaming, emotional access, and intuition. High theta may relate to impulsivity or inattention.
Alpha (8–12 Hz) – Calm Alertness
Promotes a relaxed but aware state. Low alpha may relate to anxiety; excess alpha may link to fatigue or depression.
Beta (12–38 Hz) – Active Thinking
-
- Lo-Beta: Calm focus
- Mid-Beta: Problem-solving and alertness
- Hi-Beta: Intense focus or stress
Balanced beta activity enhances productivity and attention. Too much may cause stress or over-arousal. Other measurable brainwaves include Gamma, SMR, and Mu, but training typically focuses on Delta through Hi-Beta.
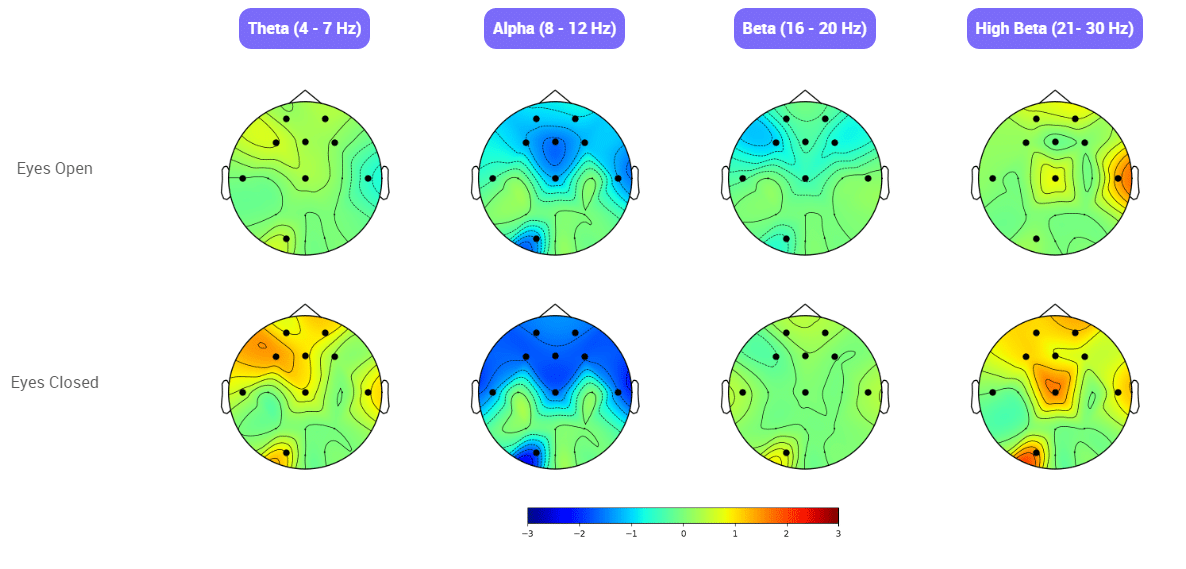
Brainwave Asymmetry and Mental Health
In a well-balanced brain, certain patterns of asymmetry are expected:
- Alpha waves are typically stronger on the left hemisphere.
- Beta waves are higher on the right hemisphere.
Imbalances in these patterns may relate to cognitive or emotional challenges. Neurofeedback aims to restore that natural balance.
What Is a Brain Map (QEEG)?
Before beginning neurofeedback, each client completes a Quantitative EEG (QEEG)—a painless, non-invasive brain scan. Your brainwave data is compared to a normative database to reveal:
- Areas of over- or under-activity
- Patterns correlated with symptoms
- A customized neurofeedback training protocol
This ensures that every client’s care is data-driven and tailored to their unique neurological profile.
Who May Benefit from Neurofeedback?
Neurofeedback can be used as a tool to help reduce symptoms associated with the following conditions. Each protocol is customized based on client needs and adjusted over time:
- Insomnia / Sleep Issues(29-33)
- Lyme Disease(34)
- Migraines and Headaches(35-38)
- Obsessive Compulsive Disorder(39-40)
- Performance Enhancement
- Post-COVID Syndrome(41)
- Post-Traumatic Stress Disorder(42-43)
- Social Anxiety Disorder(10-14)
- Traumatic Brain Injuries(44-47)
Neurofeedback is considered investigational and is not FDA-approved for the treatment of specific medical conditions. It is used as part of a wellness-based approach to support neurological regulation.
QEEG Brain Mapping
The Foundation of Personalized Neurofeedback
Before starting neurofeedback, each client completes a QEEG—also called a brain map. This painless, non-invasive scan measures the electrical patterns of your brain and compares them to a database of healthy brains.
Your results help us:
- Identify areas of over- or under-activity
- Link brainwave patterns to symptoms
- Develop a customized training protocol tailored to your needs
This evidence-based approach ensures your care is data-driven and customized from day one.
Schedule Your Brain Map Today →
How Neurofeedback Works
Neurofeedback works by monitoring your brain waves in real time and providing your brain with instant feedback. This “feedback” can take different forms depending on the person being treated. For example, a common practice is to have the client watch a movie during their session. Whenever the client’s brain waves are at the desired range, the movie plays in high quality (feedback). However, as soon as the client’s brain wave activity diverts from that optimal range, the movie starts to get blurry (more feedback).
The client’s brain starts to learn that, in order to get the movie to play in high quality, it must reach the desired pattern of brain wave activity. Your brain eventually learns to constantly function at the optimal pattern of activity as opposed to the unhealthy pattern at which it previously operated. These brainwave changes are associated with improvements in mood, cognitive function, and emotional regulation.
What Are the Benefits of Neurofeedback?
While the effects depend on the patient, condition being treated, number and frequency of of treatments. Patients who have received neurofeedback training have experienced the following benefits in as little as 10 sessions.
✓ Improved Memory
✓ Increased Focus
✓ Improved Self Regulation
✓ Better Manage Stress
✓ Improved Sleep
✓ Reduced ADHD Symptoms
✓ Reduced Anxiety
✓ Improved Depression Symptoms

Incredibly safe, non-invasive therapy with no common side effects
Highly personalized therapy that creates lasting improvements up to years after therapy ends

The Neurofeedback Process at Extivita
Each neurofeedback therapy plan at Extivita begins with a quantitative EEG (qEEG) brain map. This allows us to measure electrical activity across your brain’s regions, identify imbalances or dysregulation, and create a personalized training protocol.
qEEG findings guide how we target training sessions and allow us to monitor progress over time.
During a typical Neurofeedback session:
- Sensors are placed on the scalp to monitor brainwave activity in real time.
- You watch a video or play a game.
- Your brain receives feedback when it is operating optimally, reinforcing healthy patterns.
Over time, this retraining helps regulate mood, attention, and behavior.
Schedule Your Brain Map Today →
Home Neurofeedback
Train from the comfort of your home.
For those who need a more flexible schedule or live farther from our clinic, Home Neurofeedback is available. We provide an easy-to-use neurofeedback system and training so you can complete sessions on your own, while still being supported by Extivita staff.
✓ Neurofeedback system and sensors
✓ Remote setup support and tutorial
✓ Ongoing review and protocol adjustment by our clinicians
✓ Scheduled check-ins to monitor progress
Home Neurofeedback delivers the same quality results with added convenience and consistency.
How Home Neurofeedback Works
Getting Started
- Virtual Consultation
- Acquire necessary hardware kit.
- Complete a qEEG assessment at home.
- Schedule a virtual report of findings (ROF).
Personalized Program
- Receive a tailored neurofeedback program after the ROF.
- Choose between 4- or 6-month program options.
Training and Support
- Enjoy unlimited training sessions.
- Monthly 30-minute home Neurofeedback Coaching call.
- Regular progress data reports.
- Option for additional coaching calls.
Program Completion
- Maintenance plan guidance in the final month.
- Use Muse app for ongoing brain regulation.
Getting Started
- Virtual Consultation
- Receive your training kit
- Complete a qEEG assessment at home
- Schedule a virtual report of findings (ROF)
Personalized Program
- Receive a tailored neurofeedback program after the ROF
- Choose between 4- or 6-month program options
Training and Support
- Train as often as you’d like
- Monthly 30-minute coaching calls with our specialist
- Regular progress data reports
- Option for additional coaching calls
Program Completion
- Maintenance plan guidance in the final month
- Use Muse app for ongoing brain regulation
Get Started with Neurofeedback
Whether you’re looking to recover, refocus, or optimize brain function, our neurofeedback therapy is tailored to help you reach your goals.
Schedule Your Brain Map Today →
Frequently Asked Questions About Neurofeedback
How do I get started with Neurofeedback (new patients)?
Begin by booking a Free Personalized Wellness Visit. This one-on-one session allows you to visit our clinic, meet with a care coordinator, and discuss your health goals. You’ll complete a brief health questionnaire and learn how Neurofeedback—and other therapies like HBOT or IV therapy—may support your wellness journey.
If you choose to move forward with Neurofeedback, the next step is scheduling a dedicated session with our Neurofeedback Specialist, which includes your initial qEEG brain map and the creation of your personalized training plan.
Do I need a medical consultation before starting Neurofeedback?
Not always. Neurofeedback does not require a prescription, so most clients can begin after their Free Personalized Wellness Visit and qEEG session. However, if you’re pursuing Hyperbaric Oxygen Therapy or requesting a medically-directed treatment plan, you’ll need a Medical Review & Prescription Visit with our licensed provider.
I'm already an Extivita patient. How do I add Neurofeedback?
If you’re currently receiving services like HBOT, IV Therapy, or PEMF, you do not need to repeat the onboarding process. Simply speak with your care coordinator or contact the clinic to schedule a Neurofeedback-specific intake and qEEG mapping session.
What is Neurofeedback?
Neurofeedback is a non-invasive, drug-free therapy that trains your brain to self-regulate. It uses real-time feedback from your brainwave activity (EEG) to help improve attention, emotional regulation, sleep, and more.
During a session, you wear sensors that read your brainwaves. While watching a video or playing a game, you receive real-time feedback—like screen dimming or sound cues—when your brain enters a more optimal state. Over time, this helps reinforce healthier patterns.
What is a brain map (qEEG)?
A qEEG (quantitative electroencephalogram) records your brain’s electrical activity and compares it to normative databases. It shows which brainwave patterns may be under- or overactive and helps us design a training plan tailored to your needs.
What happens during a Neurofeedback session?
Each session includes a brief check-in, EEG sensor setup, and about 30 minutes of training. You’ll watch a video or play a game while your brain responds to subtle cues based on your brainwave activity. The full visit typically takes 45–60 minutes.
How often should I do Neurofeedback?
We recommend starting with 2–3 sessions per week, ideally with a rest day in between. As you progress, sessions may reduce to 1–2 per week.
How many sessions will I need?
Most clients begin to notice changes after 10 sessions. However, for lasting results, we recommend a full training plan of 20–40 sessions, depending on your goals and how your brain responds.
What will my Neurofeedback protocol be?
Your protocol is personalized using your qEEG, symptom profile, and clinical goals. It may also evolve as your brain adapts and progresses through the program.
Is Neurofeedback safe?
Yes. Neurofeedback is non-invasive and has minimal side effects. Some clients may feel mildly fatigued or experience a light headache after training—similar to a workout. These effects are temporary.
Is anything being put into my brain?
No. The sensors simply read your brain activity; there is no stimulation or energy applied to your brain.
Is Neurofeedback invasive?
Not at all. It’s a passive process—just sensors on your scalp reading activity. No electricity or stimulation is used.
What conditions is Neurofeedback used for?
Neurofeedback is used as an investigational therapy to support symptoms associated with conditions like ADHD, anxiety, PTSD, TBI, and more. See our full condition list above.
Note: Neurofeedback is FDA-cleared for relaxation and stress reduction. Use for specific conditions is off-label and investigational.
Where can I learn more about the science behind Neurofeedback?
We’re happy to help! Call us at (919) 354-3775 to speak with a member of our care team or see some of our recommended research references below.
Recent Neurofeedback News & Research
Neurofeedback Treatment and Posttraumatic Stress Disorder: Effectiveness of Neurofeedback on Posttraumatic Stress Disorder and the Optimal Choice of Protocol
Abstract Neurofeedback is an alternative, noninvasive approach used in the treatment of a wide range of neuropsychiatric disorders, including posttraumatic stress disorder (PTSD). Many different neurofeedback protocols and methods exist. Likewise,...
Specific effects of EEG based neurofeedback training on memory functions in post-stroke victims
Abstract: Background: Using EEG based neurofeedback (NF), the activity of the brain is modulated directly and, therefore, the cortical substrates of cognitive functions themselves. In the present study, we investigated the ability of stroke...
The mechanism of neurofeedback training for treatment of central neuropathic pain in paraplegia: a pilot study
Abstract Background: Central neuropathic pain has a prevalence of 40% in patients with spinal cord injury. Electroencephalography (EEG) studies showed that this type of pain has identifiable signatures, that could potentially be targeted by a...
References:
- D. Corydon Hammond (2011) What is Neurofeedback: An Update, Journal of Neurotherapy, 15:4, 305-336, DOI: 10.1080/10874208.2011.623090
- Marzbani, Hengameh, et al. “Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications.” Basic and Clinical Neuroscience, vol. 7, no. 2, Apr. 2016, pp. 143–58. PubMed Central, doi:10.15412/J.BCN.03070208
- Luijmes, Robin E., et al. “The Effectiveness of Neurofeedback on Cognitive Functioning in Patients with Alzheimer’s Disease: Preliminary Results.” Neurophysiologie Clinique/Clinical Neurophysiology, vol. 46, no. 3, June 2016, pp. 179–87. ScienceDirect, doi:10.1016/j.neucli.2016.05.069.
- Surmeli, Tanju, et al. “Quantitative EEG Neurometric Analysis–Guided Neurofeedback Treatment in Dementia: 20 Cases. How Neurometric Analysis Is Important for the Treatment of Dementia and as a Biomarker?” Clinical EEG and Neuroscience, vol. 47, no. 2, SAGE Publications Inc, Apr. 2016, pp. 118–33. SAGE Journals, doi:10.1177/1550059415590750.
- Jang, Jung-Hee, et al. “Beta Wave Enhancement Neurofeedback Improves Cognitive Functions in Patients with Mild Cognitive Impairment.” Medicine, vol. 98, no. 50, Dec. 2019. PubMed Central, doi:10.1097/MD.0000000000018357.
- Lavy, Yotam, et al. “Neurofeedback Improves Memory and Peak Alpha Frequency in Individuals with Mild Cognitive Impairment.” Applied Psychophysiology and Biofeedback, vol. 44, no. 1, 2019, pp. 41–49. PubMed, doi:10.1007/s10484-018-9418-0.
- Marlats, Fabienne, et al. “SMR/Theta Neurofeedback Training Improves Cognitive Performance and EEG Activity in Elderly With Mild Cognitive Impairment: A Pilot Study.” Frontiers in Aging Neuroscience, vol. 12, June 2020. PubMed Central, doi:10.3389/fnagi.2020.00147.
- Angelakis, Efthymios, et al. “EEG Neurofeedback: A Brief Overview and an Example of Peak Alpha Frequency Training for Cognitive Enhancement in the Elderly.” The Clinical Neuropsychologist, vol. 21, no. 1, Jan. 2007, pp. 110–29. PubMed, doi:10.1080/13854040600744839.
- Becerra, Judith, et al. “Neurofeedback in Healthy Elderly Human Subjects with Electroencephalographic Risk for Cognitive Disorder.” Journal of Alzheimer’s Disease, vol. 28, no. 2, IOS Press, Jan. 2012, pp. 357–67. content.iospress.com, doi:10.3233/JAD-2011-111055.
- Hammond, D. Corydon. “Neurofeedback Treatment of Depression and Anxiety.” Journal of Adult Development, vol. 12, no. 2, Aug. 2005, pp. 131–37. Springer Link, doi:10.1007/s10804-005-7029-5.
- Biriukova, E. N., et al. “P.3.041 Clinical and Neurophysiological efficacy of Neurofeedback in the Combined Therapy of Anxiety Disorders Resistant to Psychopharmacotherapy.” European Neuropsychopharmacology, vol. 15, Jan. 2005, pp. S162–63. ScienceDirect, doi:10.1016/S0924-977X(05)80337-2.
- Dadashi, Mohsen, et al. “Effects of Increase in Amplitude of Occipital Alpha & Theta Brain Waves on Global Functioning Level of Patients with GAD.” Basic and Clinical Neuroscience, vol. 6, no. 1, Jan. 2015, pp. 14–20.
- Hou, Yue, et al. “Neurofeedback Training Improves Anxiety Trait and Depressive Symptom in GAD.” Brain and Behavior, vol. n/a, no. n/a, p. e02024. Wiley Online Library, doi:https://doi.org/10.1002/brb3.2024.
- Moscovitch, David A., et al. “Frontal EEG Asymmetry and Symptom Response to Cognitive Behavioral Therapy in Patients with Social Anxiety Disorder.” Biological Psychology, vol. 87, no. 3, July 2011, pp. 379–85. PubMed, doi:10.1016/j.biopsycho.2011.04.009.
- Enriquez-Geppert, Stefanie, et al. “Neurofeedback as a Treatment Intervention in ADHD: Current Evidence and Practice.” Current Psychiatry Reports, vol. 21, no. 6, 2019. PubMed Central, doi:10.1007/s11920-019-1021-4.
- González-Castro, Paloma, et al. “Efficacy of Neurofeedback Versus Pharmacological Support in Subjects with ADHD.” Applied Psychophysiology and Biofeedback, vol. 41, no. 1, Mar. 2016, pp. 17–25. Springer Link, doi:10.1007/s10484-015-9299-4.
- Van Doren, Jessica, et al. “Sustained Effects of Neurofeedback in ADHD: A Systematic Review and Meta-Analysis.” European Child & Adolescent Psychiatry, vol. 28, no. 3, Mar. 2019, pp. 293–305. Springer Link, doi:10.1007/s00787-018-1121-4.
- van Hoogdalem, Lothar E., et al. “The Effectiveness of Neurofeedback Therapy as an Alternative Treatment for Autism Spectrum Disorders in Children: A Systematic Review.” Journal of Psychophysiology, Hogrefe Publishing, 2020, p. No Pagination Specified-No Pagination Specified. APA PsycNET, doi:10.1027/0269-8803/a000265.
- Kouijzer, Mirjam E. J., et al. “Neurofeedback Treatment in Autism. Preliminary Findings in Behavioral, Cognitive, and Neurophysiological Functioning.” Research in Autism Spectrum Disorders, vol. 4, no. 3, July 2010, pp. 386–99. ScienceDirect, doi:10.1016/j.rasd.2009.10.007.
- Kouijzer, Mirjam E. J., et al. “Long-Term Effects of Neurofeedback Treatment in Autism.” Research in Autism Spectrum Disorders, vol. 3, no. 2, Apr. 2009, pp. 496–501. ScienceDirect, doi:10.1016/j.rasd.2008.10.003.
- Kouijzer, Mirjam E. J., et al. “Neurofeedback Improves Executive Functioning in Children with Autism Spectrum Disorders.” Research in Autism Spectrum Disorders, vol. 3, no. 1, Jan. 2009, pp. 145–62. ScienceDirect, doi:10.1016/j.rasd.2008.05.001.
- Pineda, J. A., et al. “Positive Behavioral and Electrophysiological Changes Following Neurofeedback Training in Children with Autism.” Research in Autism Spectrum Disorders, vol. 2, no. 3, July 2008, pp. 557–81. ScienceDirect, doi:10.1016/j.rasd.2007.12.003.
- Trambaiolli, Lucas, et al. “Neurofeedback Training in Major Depressive Disorder: A Systematic Review of Clinical Efficacy, Study Quality and Reporting Practices.” preprint, PsyArXiv, 1 Sept. 2020. DOI.org (Crossref), doi:10.31234/osf.io/5j4wy.
- Dias, Álvaro Machado, and Adrian van Deusen. “A New Neurofeedback Protocol for Depression.” The Spanish Journal of Psychology, vol. 14, no. 1, May 2011, pp. 374–84. DOI.org (Crossref), doi:10.5209/rev_SJOP.2011.v14.n1.34.
- Hammond, D. Corydon. “Neurofeedback Treatment of Depression and Anxiety.” Journal of Adult Development, vol. 12, no. 2, Aug. 2005, pp. 131–37. Springer Link, doi:10.1007/s10804-005-7029-5.
- Terrasa, Juan L., et al. “Self-Regulation of SMR Power Led to an Enhancement of Functional Connectivity of Somatomotor Cortices in Fibromyalgia Patients.” Frontiers in Neuroscience, vol. 14, Frontiers, 2020. Frontiers, doi:10.3389/fnins.2020.00236.
- Wu, Yu-Lin, et al. “Effects of Neurofeedback on Fibromyalgia: A Randomized Controlled Trial.” Pain Management Nursing, Feb. 2021. ScienceDirect, doi:10.1016/j.pmn.2021.01.004.
- Kayiran, Sadi, et al. “Neurofeedback Intervention in Fibromyalgia Syndrome; a Randomized, Controlled, Rater Blind Clinical Trial.” Applied Psychophysiology and Biofeedback, vol. 35, no. 4, Dec. 2010, pp. 293–302. PubMed, doi:10.1007/s10484-010-9135-9.
- Arns, Martijn, et al. “Differential Effects of Theta/Beta and SMR Neurofeedback in ADHD on Sleep Onset Latency.” Frontiers in Human Neuroscience, vol. 8, Dec. 2014. PubMed Central, doi:10.3389/fnhum.2014.01019.
- Schabus, Manuel, et al. “Enhancing Sleep Quality and Memory in Insomnia Using Instrumental Sensorimotor Rhythm Conditioning.” Biological Psychology, vol. 95, Jan. 2014, pp. 126–34. ScienceDirect, doi:10.1016/j.biopsycho.2013.02.020.
- Hammer, Barbara U., et al. “Neurofeedback for Insomnia: A Pilot Study of Z-Score SMR and Individualized Protocols.” Applied Psychophysiology and Biofeedback, vol. 36, no. 4, Dec. 2011, pp. 251–64. PubMed, doi:10.1007/s10484-011-9165-y.
- Cortoos, Aisha, et al. “An Exploratory Study on the Effects of Tele-Neurofeedback and Tele-Biofeedback on Objective and Subjective Sleep in Patients with Primary Insomnia.” Applied Psychophysiology and Biofeedback, vol. 35, no. 2, June 2010, pp. 125–34. DOI.org (Crossref), doi:10.1007/s10484-009-9116-z.
- Perlis, Michael L., et al. “Beta/Gamma EEG Activity in Patients with Primary and Secondary Insomnia and Good Sleeper Controls.” Sleep, vol. 24, no. 1, Jan. 2001, pp. 110–17. Silverchair, doi:10.1093/sleep/24.1.110.
- Brown, Valdeane. “Neurofeedback and Lyme’s Disease:” Journal of Neurotherapy, vol. 1, no. 2, Routledge, Aug. 1995, pp. 60–73. Taylor and Francis+NEJM, doi:10.1300/J184v01n02_05.
- Kosari, Zahra, et al. “Comparing the Effectiveness of Neurofeedback and Transcranial Direct Current Stimulation on Sleep Quality of Patients With Migraine.” Basic and Clinical Neuroscience, vol. 10, no. 6, 2019, pp. 579–88. PubMed Central, doi:10.32598/BCN.10.6.651.3.
- Walker, Jonathan E. “QEEG-Guided Neurofeedback for Recurrent Migraine Headaches.” Clinical EEG and Neuroscience, vol. 42, no. 1, SAGE Publications Inc, Jan. 2011, pp. 59–61. SAGE Journals, doi:10.1177/155005941104200112.
- Stokes, Deborah A., and Martha S. Lappin. “Neurofeedback and Biofeedback with 37 Migraineurs: A Clinical Outcome Study.” Behavioral and Brain Functions : BBF, vol. 6, Feb. 2010, p. 9. PubMed Central, doi:10.1186/1744-9081-6-9.
- Siniatchkin, M., et al. “Self-Regulation of Slow Cortical Potentials in Children with Migraine: An Exploratory Study.” Applied Psychophysiology and Biofeedback, vol. 25, no. 1, Mar. 2000, pp. 13–32. PubMed, doi:10.1023/a:1009581321624.
- Hammond, Corydon. “QEEG-Guided Neurofeedback in the Treatment of Obsessive Compulsive Disorder.” Journal of Neurotherapy, vol. 7, no. 2, Routledge, Mar. 2003, pp. 25–52. Taylor and Francis+NEJM, doi:10.1300/J184v07n02_03.
- Hammond, D. Corydon. “Neurofeedback with Anxiety and Affective Disorders.” Child and Adolescent Psychiatric Clinics of North America, vol. 14, no. 1, Jan. 2005, pp. 105–23, vii. PubMed, doi:10.1016/j.chc.2004.07.008.
- Luctkar-Flude, Marian, and Dianne Groll. “A Systematic Review of the Safety and Effect of Neurofeedback on Fatigue and Cognition.” Integrative Cancer Therapies, vol. 14, no. 4, SAGE Publications Inc STM, July 2015, pp. 318–40. SAGE Journals, doi:10.1177/1534735415572886.
- Kolk, Bessel A. van der, et al. “A Randomized Controlled Study of Neurofeedback for Chronic PTSD.” PLOS ONE, vol. 11, no. 12, Public Library of Science, Dec. 2016, p. e0166752. PLoS Journals, doi:10.1371/journal.pone.0166752.
- Reiter, Karen, et al. “Neurofeedback Treatment and Posttraumatic Stress Disorder: Effectiveness of Neurofeedback on Posttraumatic Stress Disorder and the Optimal Choice of Protocol.” The Journal of Nervous and Mental Disease, vol. 204, no. 2, Feb. 2016, pp. 69–77. journals.lww.com, doi:10.1097/NMD.0000000000000418.
- Bennett, Cathlyn N., et al. “Clinical and Biochemical Outcomes Following EEG Neurofeedback Training in Traumatic Brain Injury in the Context of Spontaneous Recovery.” Clinical EEG and Neuroscience, vol. 49, no. 6, Nov. 2018, pp. 433–40. PubMed, doi:10.1177/1550059417744899.
- Munivenkatappa, Ashok, et al. “EEG Neurofeedback Therapy: Can It Attenuate Brain Changes in TBI?” NeuroRehabilitation, vol. 35, no. 3, IOS Press, Jan. 2014, pp. 481–84. content.iospress.com, doi:10.3233/NRE-141140.
- Reddy, Rajakumari P, et al. “Neurofeedback Training to Enhance Learning and Memory in Patient with Traumatic Brain Injury: A Single Case Study.” The Indian Journal of Neurotrauma, vol. 6, no. 1, June 2009, pp. 87–90. ScienceDirect, doi:10.1016/S0973-0508(09)80037-3.
- Reddy, Rajakumari Pampa, et al. “Silent Epidemic: The Effects of Neurofeedback on Quality-of-Life.” Indian Journal of Psychological Medicine, vol. 36, no. 1, 2014, pp. 40–44. PubMed Central, doi:10.4103/0253-7176.127246.